https://sites.google.com/a/umich.edu/bluelink/resources/bluelink
Labels
- Home
- Openstax Ebook
- Socratic Biology
- Learn Genetics
- Immune system
- National library of medicine
- Osteogenesis Imperfecta
- The Biology of Cancer
- Glossary of Terms social Justice
- Shelf Stable Food Safety
- Biology Dictionary
- Jeff Schinske Google scholor
- Michigan School of medicine
- Lab stimulation
- Biology 40A
Thursday, June 27, 2024
Lab safety
Biology Lab Safety - Foothill College
Laboratory Safety Guidelines
Note: Your instructor may have additional requirements for your specific lab
EMERGENCY INSTRUCTIONS
Campus Safety Information: http://www.foothill.fhda.edu/staff/safetyscript.phpLinks to an external site.
- Earthquake – In case of an earthquake, turn off all gas and water valves, stay inside, and get under a table or bench. Stay away from glass, windows, and objects that may fall from high places. Do not stand in any doorway that has a door.
- Fire – In case of fire, notify a faculty or staff member Stay calm. All classrooms are equipped with at least one fire extinguisher located next to an exterior door. Fire alarms are located adjacent to the exterior doors on the west side of the building (in the Stock Room).
- Campus Fire Alarm Activation – In the event of a fire or bomb threat, a campus-wide alarm will
- Stay Leave all loose items, including books, bags, and umbrellas, in the classroom and proceed down the stairs to Parking Lot 8.
- Evacuation routes are posted near the exterior doors of each
- Do not use the elevators.
- Your instructor or the Lab Technician will lock the doors after everyone is
- Do not stay in or near the
- You will be told when it is safe to return, and no one will be allowed to re-enter the classroom until that time.
- Threat of Shooting – If it is suspected that a gunman might be threatening the campus, a phone tree/e-mail system is The policy in the event of an active shooter is to Run - Hide - Fight. If you can safely get away, do so and take cover. If you cannot escape, hide (lock doors, turn off lights, remain quiet to give the illusion of an empty classroom). If you cannot run or hide, commit to fighting.
GENERAL LABORATORY INSTRUCTIONS
- Foodstuffs – Eating (including chewing gum), drinking, and smoking are not allowed in any No visible food or drink containers are allowed in the lab.
- Working in the Lab – No one is permitted to work in the lab without supervision by an authorized individual. Unauthorized experiments are Labs for use only by students enrolled in laboratory classes. You are not allowed into the support areas (stock room, microscope room culture room, tissue culture room, etc.) unless specifically invited to be there by a staff or faculty member. Children are never allowed in the lab.
- Safety Equipment – Safety showers and eyewashes are located throughout the Your instructor will show you where to find the nearest units and show you how to use them.
- Eye Protection – Students may be required to wear appropriate eye protection in the lab. You are advised against wearing contact lenses in the lab. However, if you need to wear them, it is your responsibility to inform the instructor and/or emergency response personnel in case of injury to the
- Footwear – You are advised to wear closed-toed and closed-heeled shoes at all times Sandals, flip-flops, or clogs should not be worn in the lab.
- Hair – Long hair should be tied back at all Remember that hair spray is flammable. Even short hair should be kept away from any source of flame.
- Clothing – Many labs require a lab It should be loose fitting and provide protection from neck to knees. Avoid floppy sleeves.
- Hygiene and Cleanliness –
- Wash your hands before beginning the lab and again before you leave. Do not apply cosmetics in the lab.
- Do not adjust or clean contact lenses in the
- Keep your hands and pencils or pens away from your eyes, nose, and mouth. Clean your lab bench before the beginning of the lab and again at the end of any “wet” lab (“wet” labs are those that use animals, chemicals, microorganisms, or any fluids).
- At the end of the lab, rinse any glassware or other equipment (spoons, cutting boards, knives, garlic presses, dissecting instruments, ), dry the equipment, and put it back where it was at the beginning of the lab
- Leave your bench and the counters neat and clean and free from any spills
- Gas Valve Use – Be certain that gas valves are closed completely when not in use. If you think you smell gas, inform your instructor or a staff member There are emergency shut-off valves located in each lab.
- Injuries – All injuries (even minor ones) must be reported to your instructor
- Spills and Breakage – Notify your instructor immediately if you spill or break All spills must be logged into a record and your instructor will take care of that. Do not work with broken or cracked glassware.
- Equipment Care – Do not carry equipment to any other area unless asked to do so by a staff or faculty Inform your instructor immediately if any piece of equipment fails to operate as expected. Always ask for more training if you are unsure about the operation of a piece of equipment.
- Microscope Care – Please see separate instructions for the microscope
INFORMATION ITEM
- MSDS (Manufacturer’s Safety Data Sheets) – Most labs do not require students to use an If you do need them, the MSDS binders are located in the Stock Room, mounted on the west wall. Above them is a poster explaining their use, but please feel free to ask questions about anything that isn’t clear to you.
DENIAL OF LAB PRIVILEGES
- Lab privileges may be denied to anyone who does not act under safe laboratory
Lab Practical 2
Lab Practical 2
- Due No Due Date
- Points 50
- Submitting on paper
Information for Lab Practical
Logistics:
- Walk-in and leave backpacks on the counter. No phones are allowed to be out during the practical. No smart watches either. If I see them then you will get an automatic zero (0) grade for the practical
- Stand at a space where there is a colored exam. Do not start until I give the order to start.
- No talking will be allowed during the practical. You may only ask me for clarifying questions but that is about it.
- You are not allowed to touch the models, only see them with your eyes.
- Microscopes: You may only use the fine focus knob to adjust the microscope. Do not move the microscope otherwise, leave them where they are sitting. If you need it adjusted, call me over.
- You will be given two (2) rounds to look at the questions. The first round will last 90 seconds. The second round will last 45 seconds. Once the timer has gone off, then you must move on.
- If you are at station 26, the next question will be at station 1 across the room.
- Follow the questions in numerical order.
- Once we are done, turn in your answer sheet and you may exit the room.
- Bathroom: Please use the bathroom before entering the lab room. Leaving the practical is not allowed, if you choose to leave then you must turn in your practical, and you are done.
- Be on time!!! Once the doors close, they will not open again until the practical is over.
- Make sure you arrive at your own time slot. Do not arrive at the opposite time slot.
Female Reproductive System Histology
Female Reproductive System Histology
Female Reproductive System Lab
Learning Objectives
- Explain the regular progression of follicular development and atresia occurring in a cyclic fashion in the primary ovary
- Describe the structural changes that occur in the uterus over the course of the menstrual cycle and pregnancy
- Characterize the histological features of the oviduct, uterus, cervix, and vagina, with particular attention to the mucosal linings of these tissues
Pre-Lab Reading
Introduction
The female reproductive system is unique in that its histological appearance cycles and undergoes structural changes that are not pathological. This laboratory will focus on the female reproductive system throughout the course of the menstrual cycle and pregnancy. It is necessary to have a conceptual understanding of the changes that occur in the ovary and uterus during these events so that the histological findings can be understood in the context of reproductive physiology.
Overview of the Female Reproductive System
The female reproductive system is composed of two gonads known as ovaries, two oviducts, the uterus, the vagina and external genitalia, and two mammary glands. Its development, maturation, and functioning is dependent upon a complex interplay of hormones from the hypothalamus, pituitary gland, adrenal glands, ovaries, and placenta.
The system has six primary functions:
- Produce ova via oogenesis
- Receive spermatozoa
- Provide an environment for fertilization
- Provide an environment for fetal development
- Expel the developed fetus
- Provide nutrition to the newborn
Ovary
The human ovary consists of an inner medulla and outer cortex with indistinct boundaries. The medulla contains the blood vessels and nerves, while the cortex is occupied by developing follicles. Visible in this ovary are follicles in various stages of development. Also visible is a corpus luteum, the remnants of a follicle that has burst and sent its ovum into the genital tract. 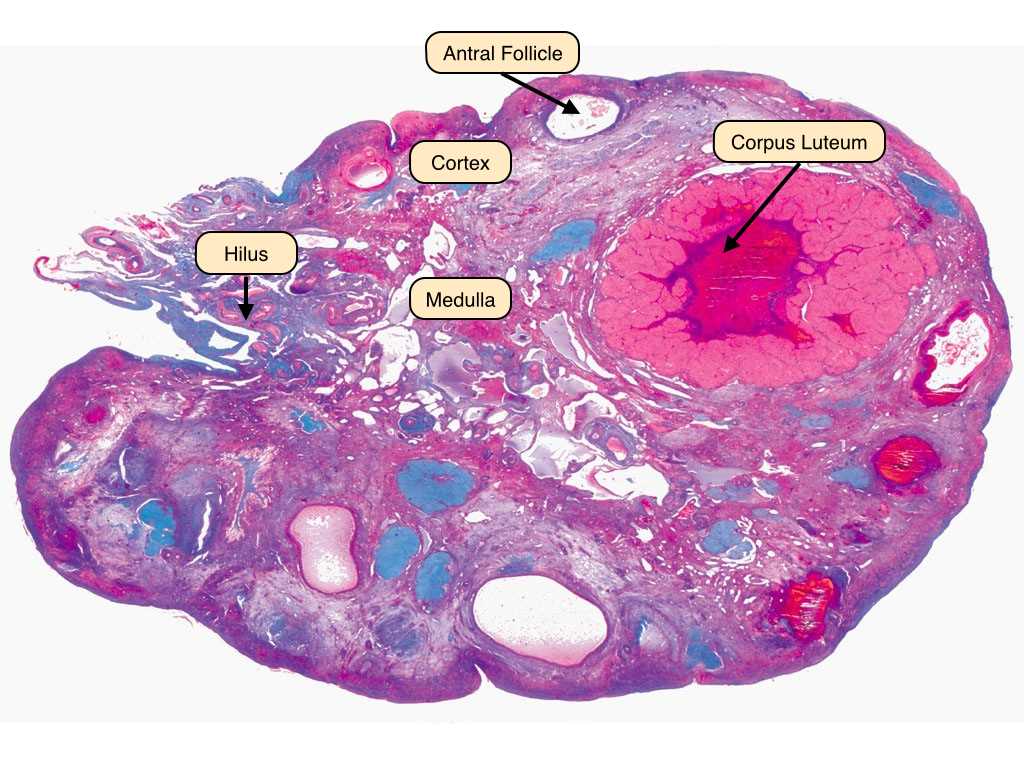
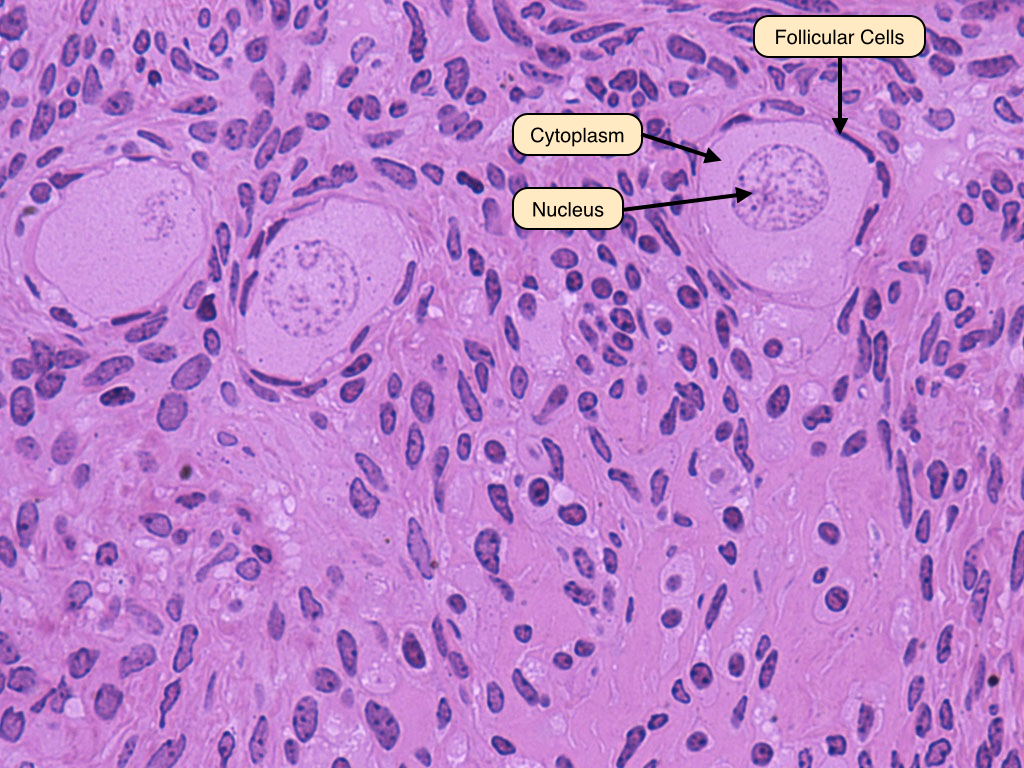
Primordial Follicles
An ovarian follicle progresses through several distinct phases before it releases its ovum. During the first five months of development, a finite number of primordial follicles form in the fetal ovary. These follicles consist of oocytes surrounded by a single layer of squamous follicular cells. These primordial follicles remain in the process of the first meiotic division. At puberty, they begin to develop further and become primary follicles.
Early Primary Follicle
The primary follicle has a central oocyte and is surrounded by a single layer of cuboidal cells. The zona pellucida is a thin band that separates these two layers. 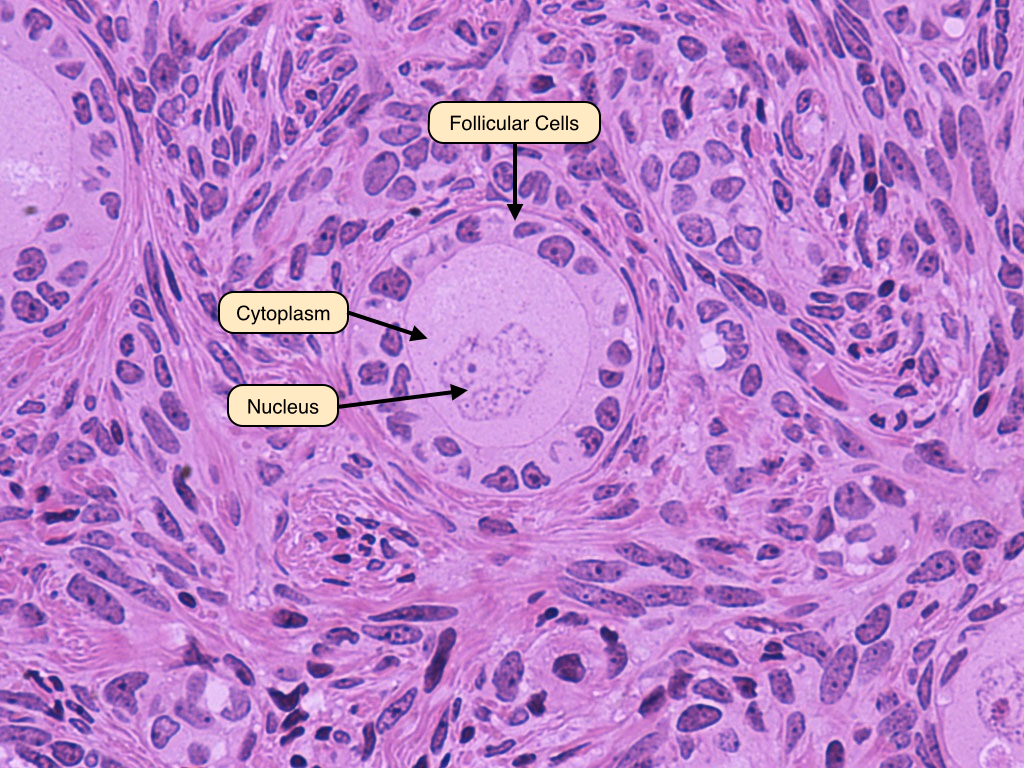
Late Primary Follicle
The late primary follicle stage is achieved when the follicular cells proliferate into a stratified epithelium known as the zona granulosa. The zona pellucida can be seen even more clearly in this image. 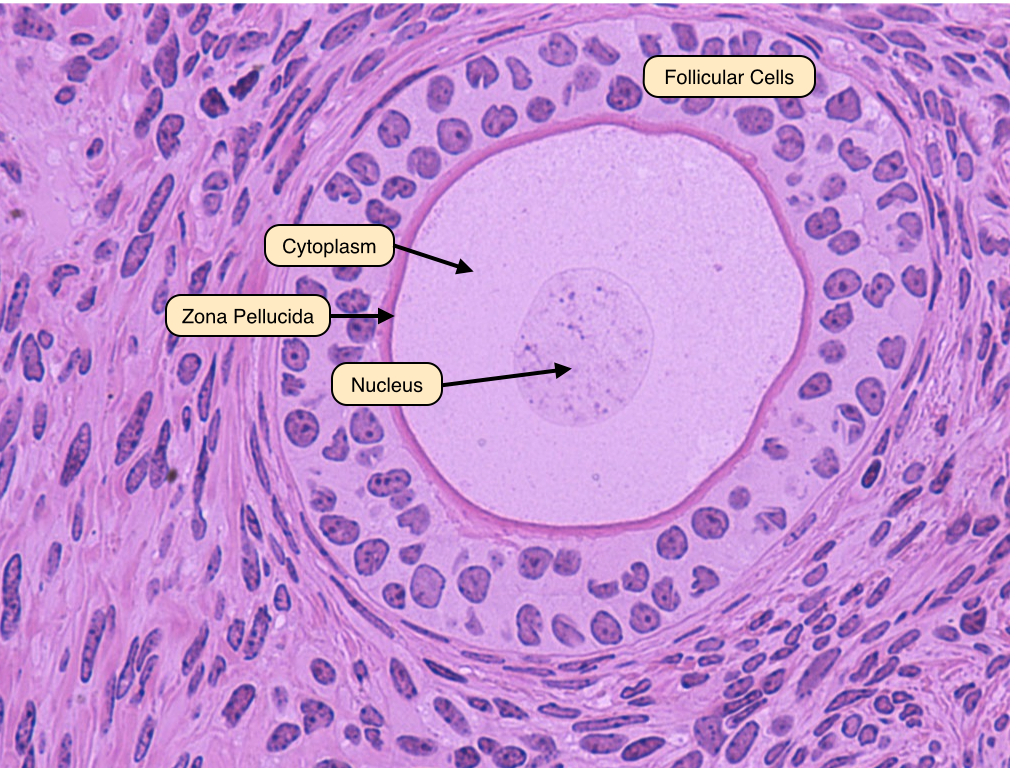
Secondary Follicle
The characteristic feature that distinguishes secondary from primary follicles is the appearance of a follicular antrum within the granulosa layer. This gap contains fluid known as liquor folliculi. Also visible in this image are the oocyte and the zona pellucida. The follicle is surrounded by the theca interna, whose cells produce hormones. 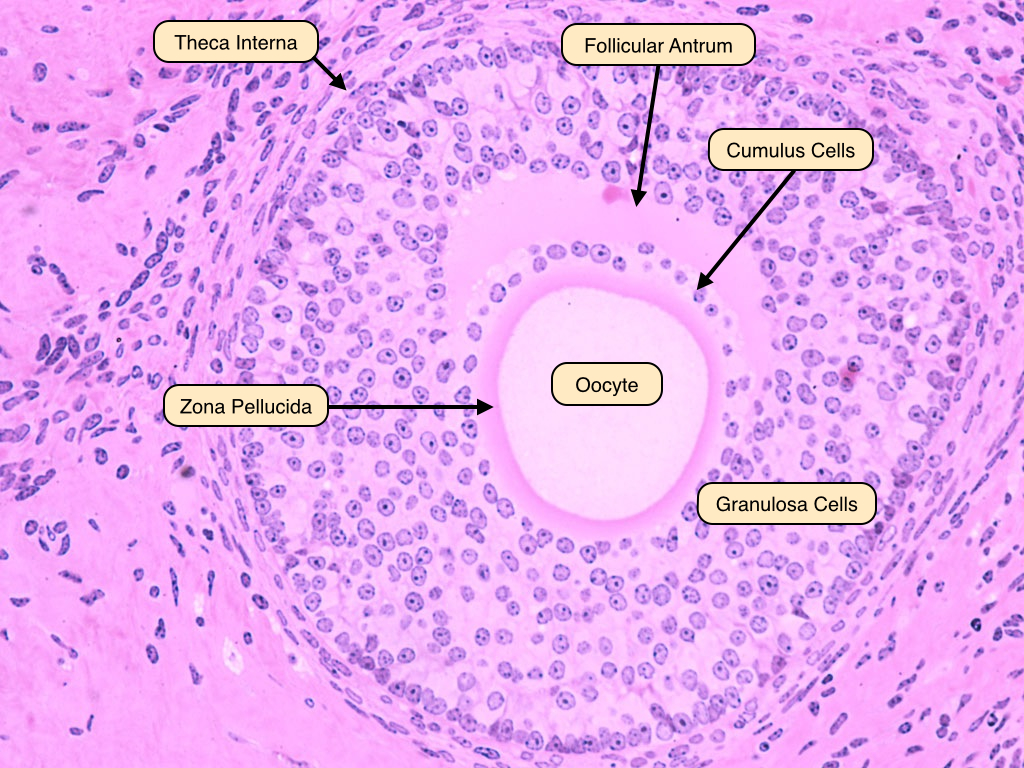
Graafian Follicle
The Graafian follicle is the follicular stage after the first meiotic division but before ovulation. It therefore contains a 2N haploid oocyte. It is characterized by a large follicular antrum that makes up most of the follicle. The secondary oocyte, having undergone the first meiotic division, is located eccentrically. It is surrounded by the zona pellucida and a layer of several cells known as the corona radiata. When released from the Graafian follicle and into the oviduct, the ovum will contain three layers: oocyte, zona pellucida and corona radiata. 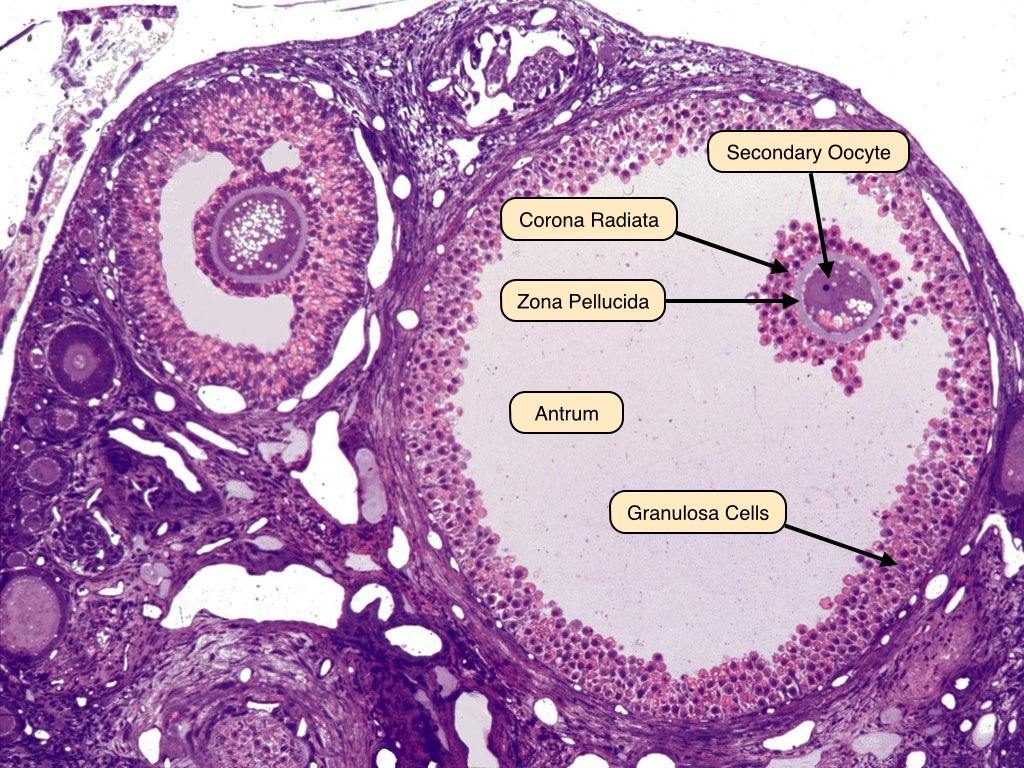
Corpus Luteum
The corpus luteum is the endocrine remains of the collapsed follicle. The center contains the remains of the blood clot that formed after ovulation. Surrounding the clot are glanulosa lutein cells and on the outside theca lutein cells.

Lutein Cells
The granulosa lutein cells have an appearance characteristic of steroid-producing cells, with pale cytoplasm indicating the presence of lipid droplets. Theca lutein cells are smaller and more deeply stained. If fertilization and implantation ensue, the corpus luteum will be maintained by hCG and remain active as the corpus luteum of pregnancy. 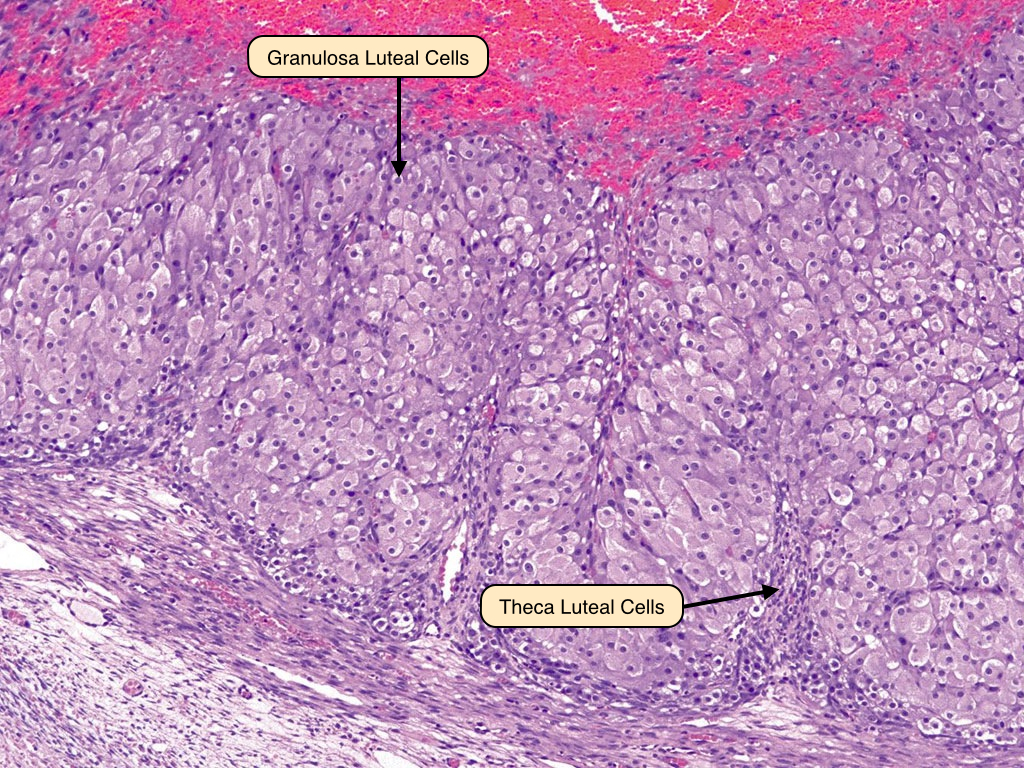
Corpus Albicans
If fertilization does not occur, the corpus luteum involutes to form the corpus albicans that is filled with fibrous tissue. The secretory cells of the corpus luteum degenerate and are phagocytoses by macrophages. 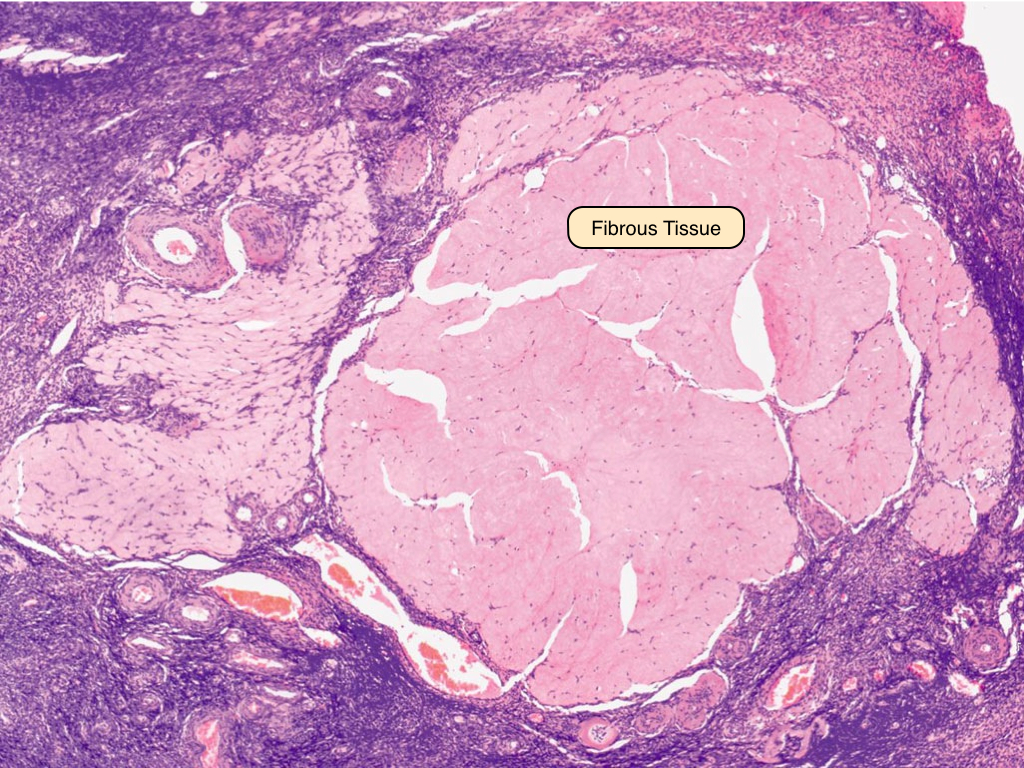
Atretic Follicle
Degeneration of follicle (atresia) can occur at any stage of development. The granulosa cells undergo apoptosis and consequently, the oocyte degenerates. The basement that separated the oocyte from granulosa cells often thickens to become the glassy membrane. Fibrous material replaces the granulosa cells. 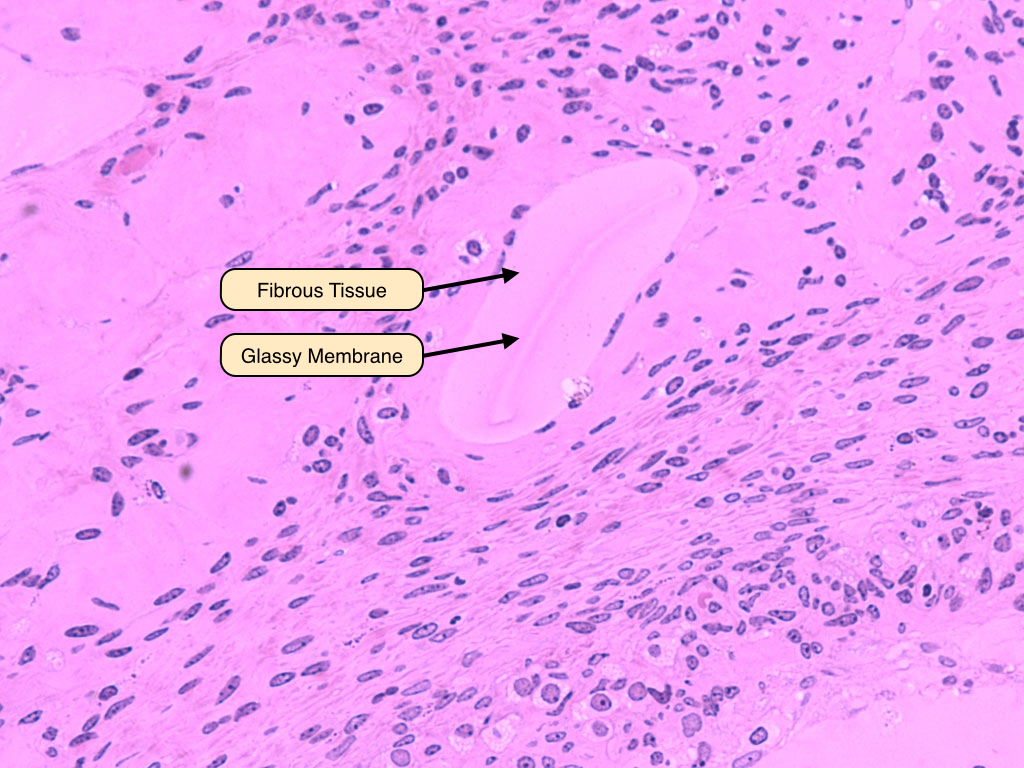
Oviduct
The oviduct consists of several segments: the infundibulum, which contains fimbriae and is located adjacent to the ovary, the ampulla, the isthmus, and the pars interstitialis. The first two of these regions have a characteristic appearance that is dominated by an elaborate mucosa that is thrown into numerous branched folds, surrounded by a relatively thin layer of smooth muscle. As the tube moves away from the ovary and toward the uterus, these folds become smaller and the smooth muscle dominates. 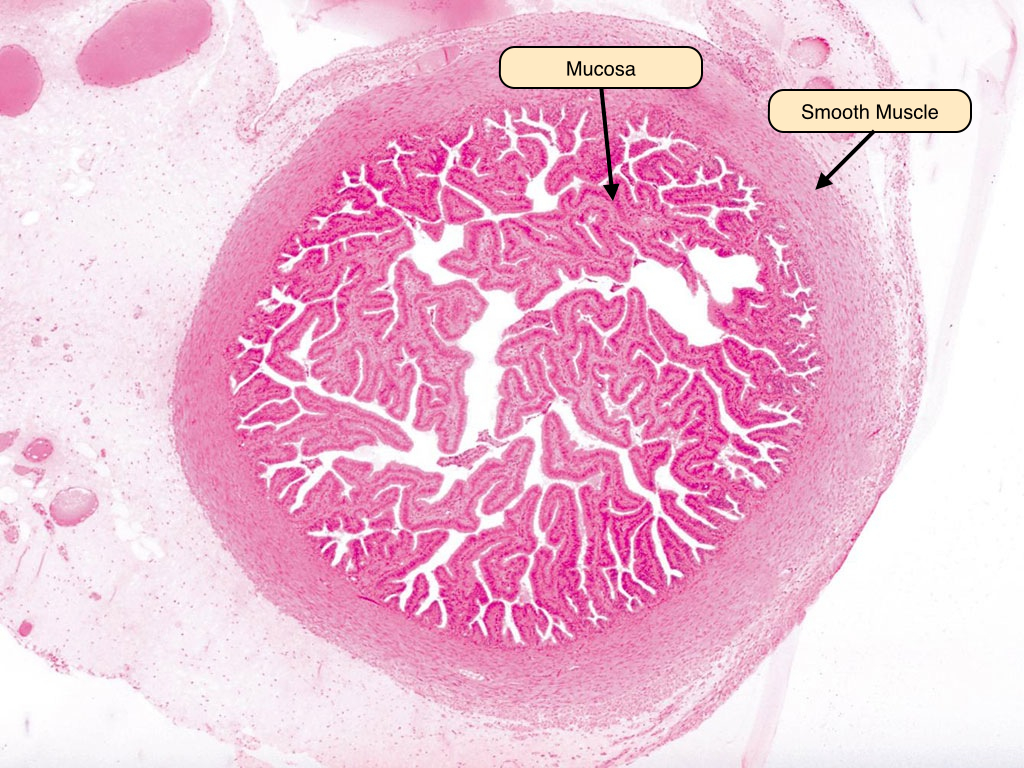
Oviduct Epithelium
The oviduct epithelium consists of two distinct cell types. The ciliated cells dominate and serve to move the ovum away from the ovary and toward the uterus. The non-ciliated secretory cells, also known as peg cells, release a secretion that lubricates the tube and provides nourishment and protection to the traveling ovum. 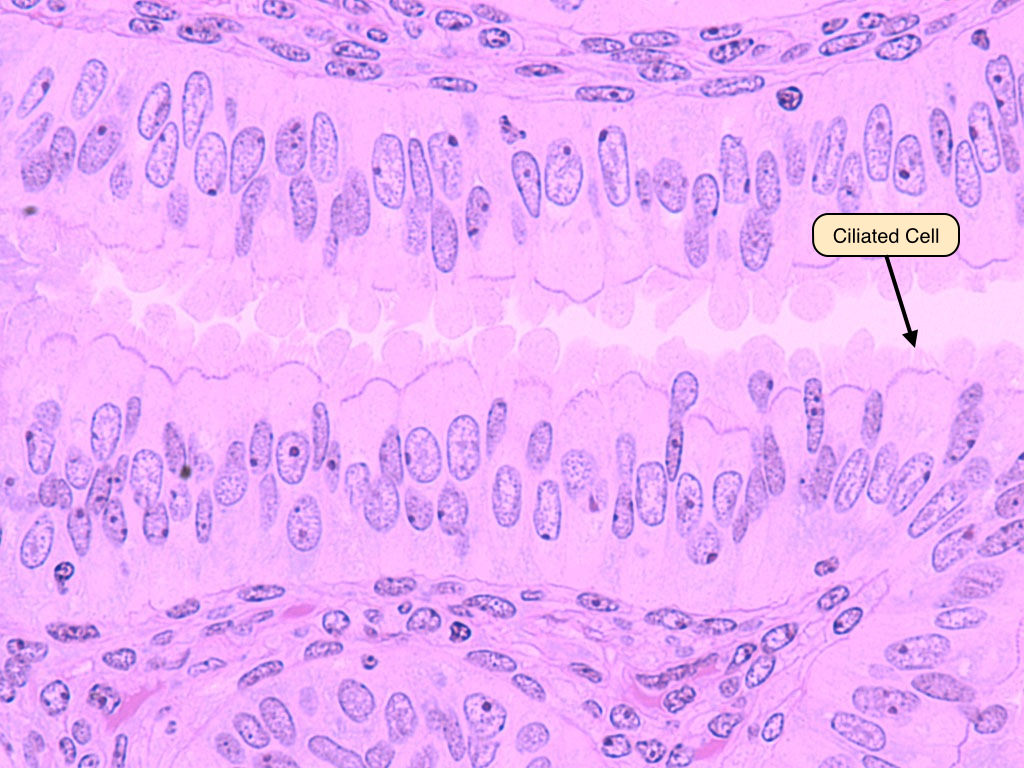
Uterus
The uterus is divided into several layers that have distinct structural and functional characteristics. The simplest classification of these layers is their division into a mucosal layer, or endometrium, a muscularis layer, or myometrium, and a serosal layer, or perimetrium. The endometrium itself is divided into two layers, the stratum functionalis and stratum basalis. During the menstrual cycle, the stratum functionalis expands and vascularizes and is subsequently sloughed off during the process of menstruation, whereas the stratum basalis remains relatively constant. The myometrium allows for the expansion and contraction of the uterine cavity and is responsive to the hormone oxytocin. 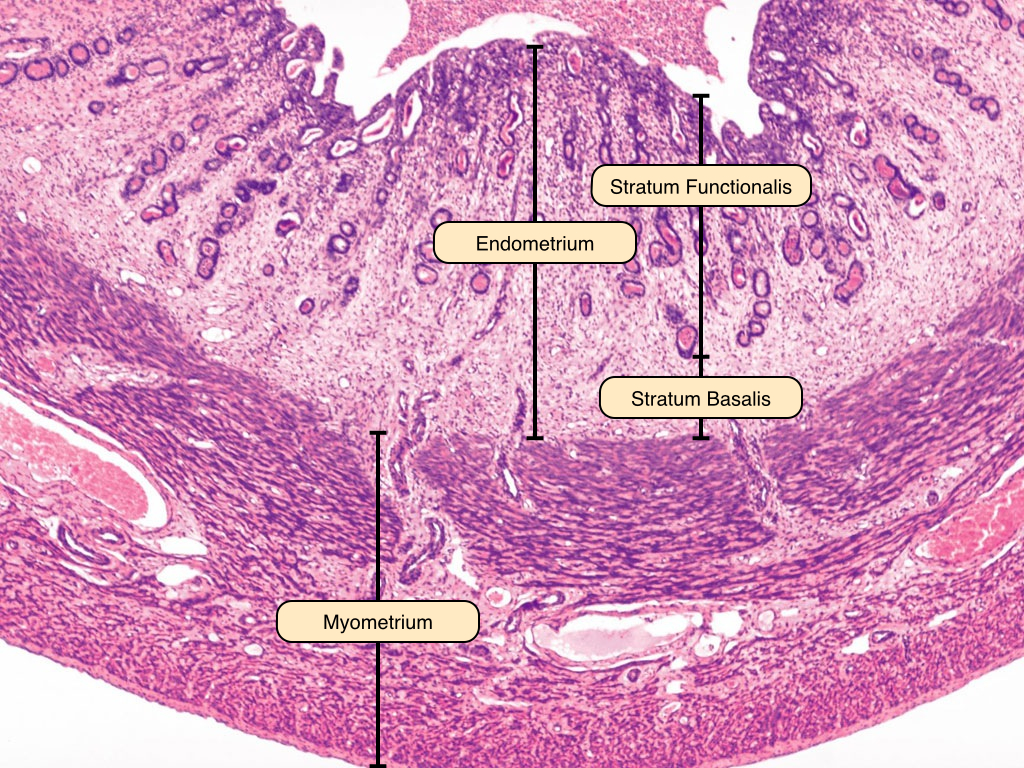
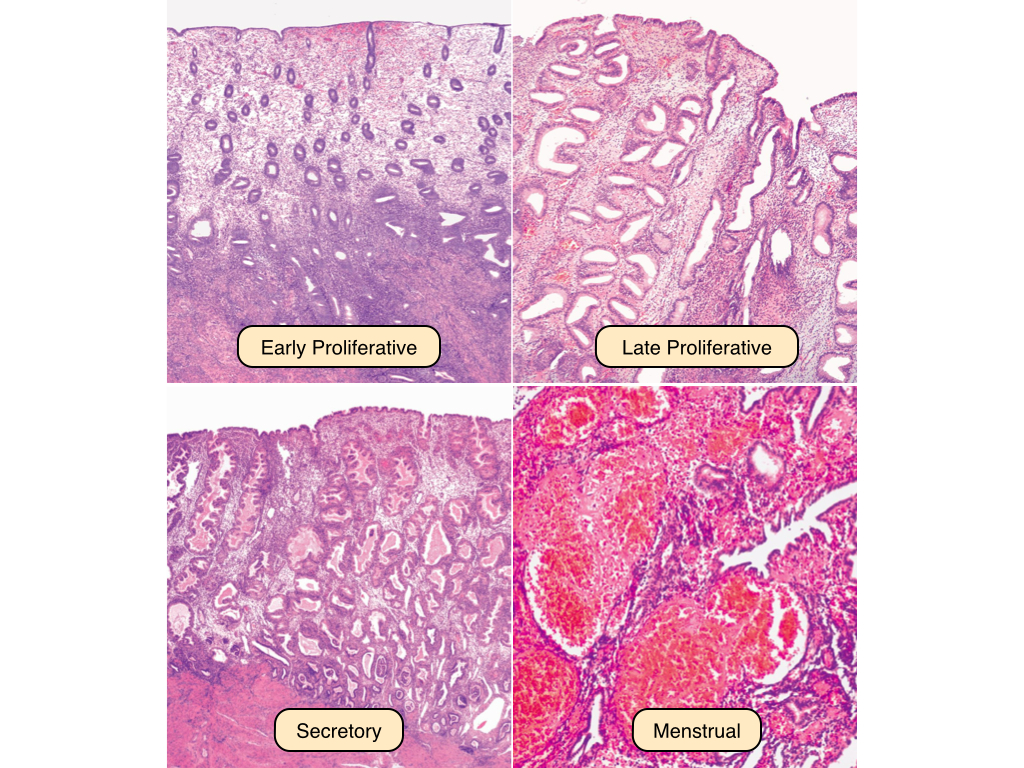
Uterine Cycle
The early proliferative phase of the uterine cycle begins at the end of menstrual flow. The uterine glands in this phase are sparse and relatively small, and the epithelial cells develop microvilli and cilia under the influence of estrogen. The late proliferative phase reveals an increased thickness of the stratum functionalis, and the glands are more coiled and densely packed. The secretory phase of the uterine cycle begins at ovulation. In this phase, the glands become even more complexly coiled and the endometrial lining reaches its maximal thickness, whereas the stratum basalis and myometrium remain relatively unchanged. Note the saw-toothed appearance of the glands. Secretions rich in glycogen and glycoprotein can be observed in the lumina of the glands. If fertilization does not occur, the placental tissue does not produce hCG and the corpus luteum degenerates. The uterine lining does not receive the progesterone, causing the spiral arteries constrict and the endometrial tissue to become ischemic. This causes cell death and the sloughing of the stratum functionalis.
Cervix
The cervix lies at the base of the uterus and serves to protect it from bacterial infiltration. It is the site of an important epithelial transition. The upper cervix (endocervix) is lined by a simple columnar epithelium that contains mucous-secreting cells. In contrast, the lower cervix (ectocervix) is lined by a stratified squamous epithelium. The transition point between these two epithelia is known as the external os. Note how the underlying layers of the cervix are composed primarily of collagenous and elastic connective tissue rather than smooth muscle fibers. 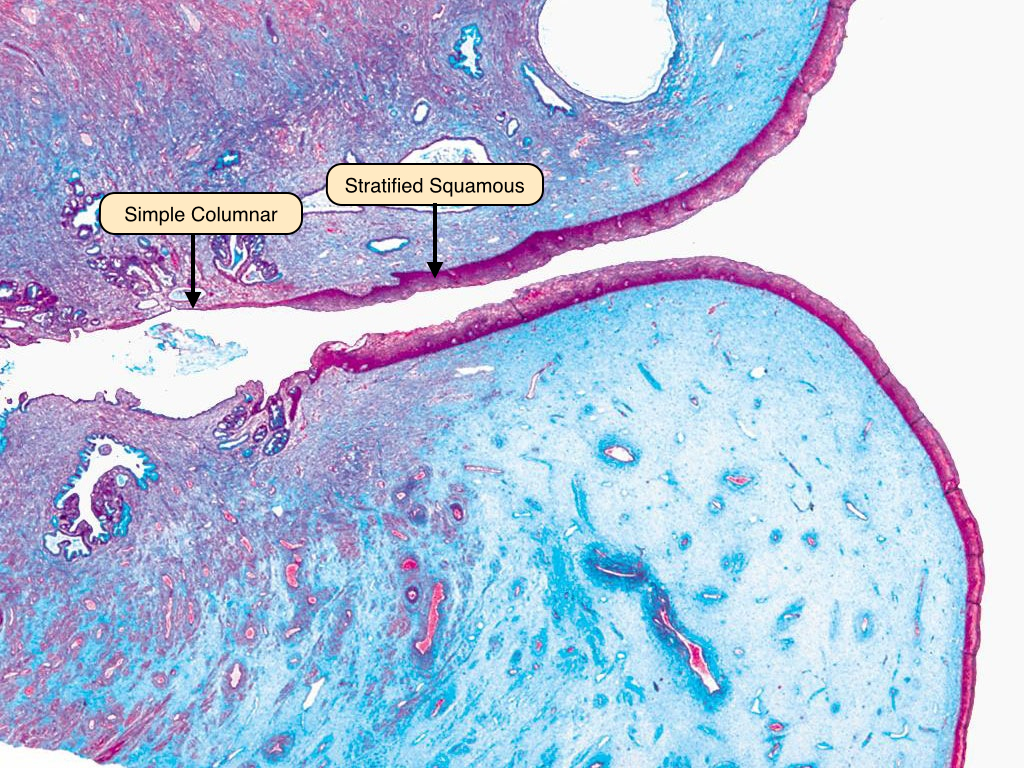
Vagina Epithelium
The vagina is lined by a stratified squamous epithelium that features a small degree of keratinization. Below the epithelium is a thick layer of dense connective tissue, like that in the dermis of the skin. A layer of loose connective tissue containing many blood vessels and nerves follows this. The cells of the vaginal wall typically contain a relatively large amount of cytoplasm because they produce and store glycogen. 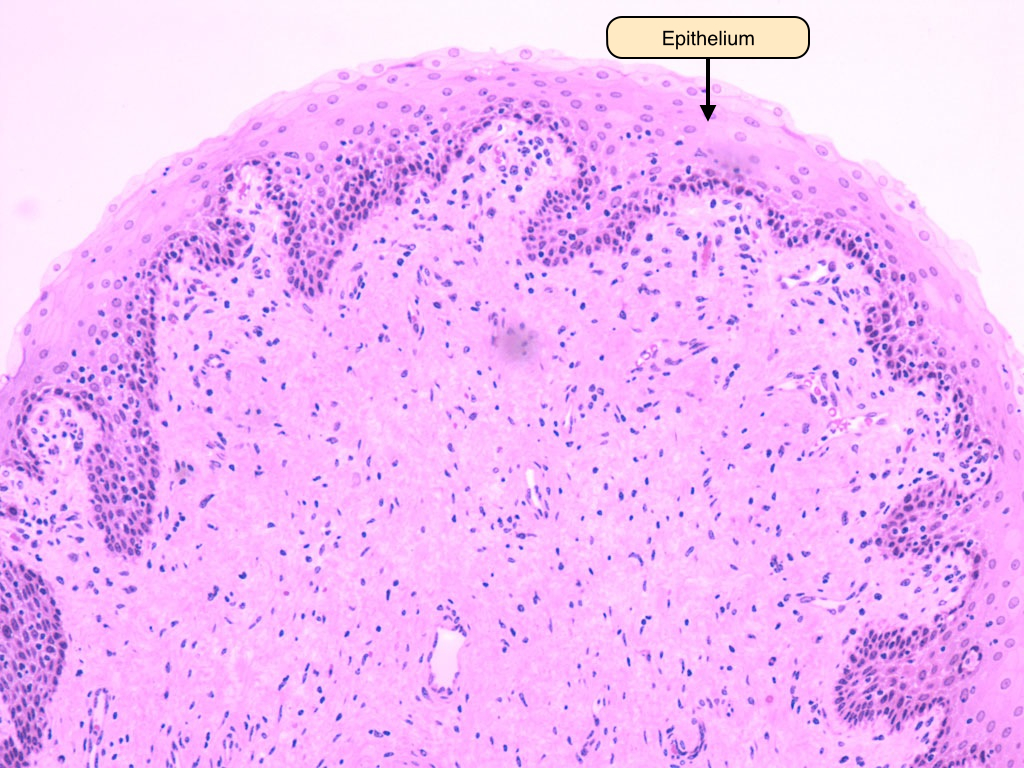
week 7 Male Reproductive System Histology
Male Reproductive System Histology
Male Reproductive System Lab
Learning Objectives
- Describe the histological organization of the testis and the process of spermatogenesis in the germinal epithelium of the seminiferous tubule
- Contrast spermatogenesis from spermiogenesis
- Draw a sperm cell and label its major parts
- Explain the importance of each portion of the duct system and accessory glands of the male reproductive tract
- Explain the structural and functional significance of the blood-testis barrier
- Describe the structure and function of the prostate gland
Pre-Lab Reading
Introduction
The male reproductive system can be thought of as a series of tubes. These tubes deliver the male gametes from their site of production in the testes to their destination outside the body. The system itself is divided into two distinct units: testes, located outside the major body cavity and housed in the scrotum and the excretory duct system, which transports the sperm from the testes and whose accessory glands produce and modify the contents of semen.
Testes
The testes are a source of gametes and steroid sex hormones. It is encapsulated by the fibrous tunica albuginea and tunica vasculosa (not visible here). Septa extending inwards from the tunica albuginea partition the gland into lobules. The bulk of the gland is composed of the seminiferous tubules, in which sperm develop. After exiting the testicular duct system composed of the rete testis and ductus efferentes, spermatozoa enter the highly convoluted epididymis, visible on the dorsal aspect of the testis here. 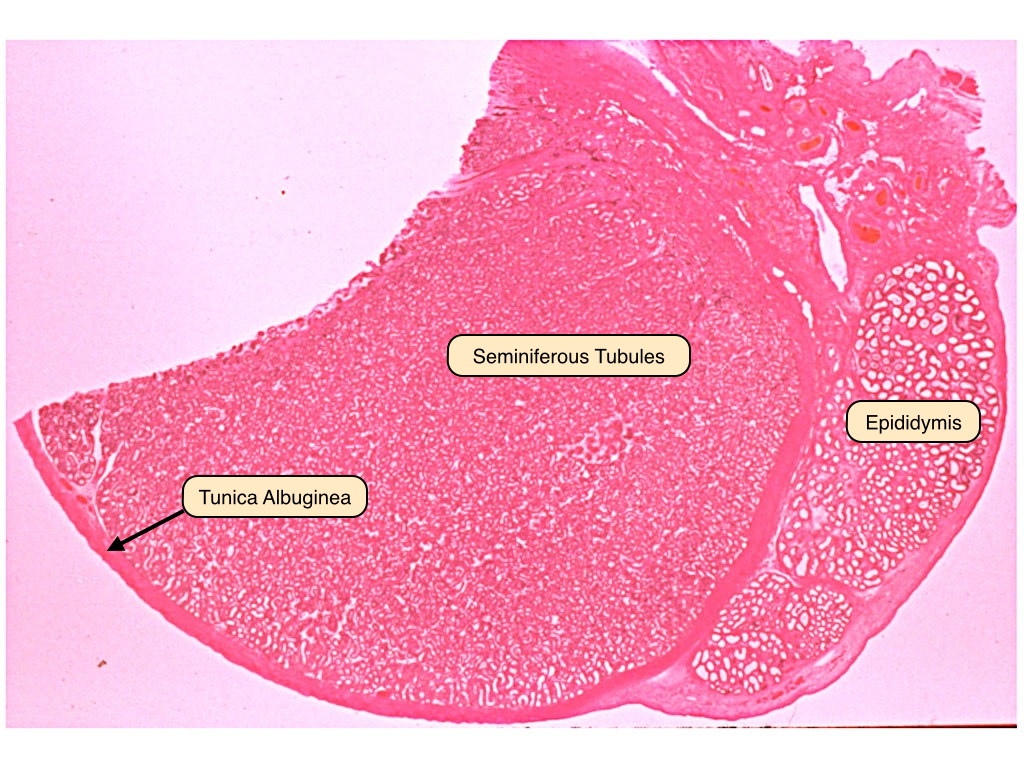
Seminiferous Tubules
Spermatozoa are produced in the germinal epithelium of the seminiferous tubules and released into the lumina of these ducts. The germinal epithelium contains both Sertoli cells and the developing spermatocytes. Sertoli cells extend from the basement membrane of the germinal epithelium to the lumen of the tubule. These cells envelope the developing sperm cells. They are joined to one another by junctional complexes and form the blood-testis barrier. The interstitial space contains clumps of darker, eosinophilic cells. These are the Leydig cells, which produce and release testosterone. Myoid cells surround the tubules and generate rhythmic contractions to propel spermatozoa and fluid. They also synthesize collagen and other fibers of connective tissue. 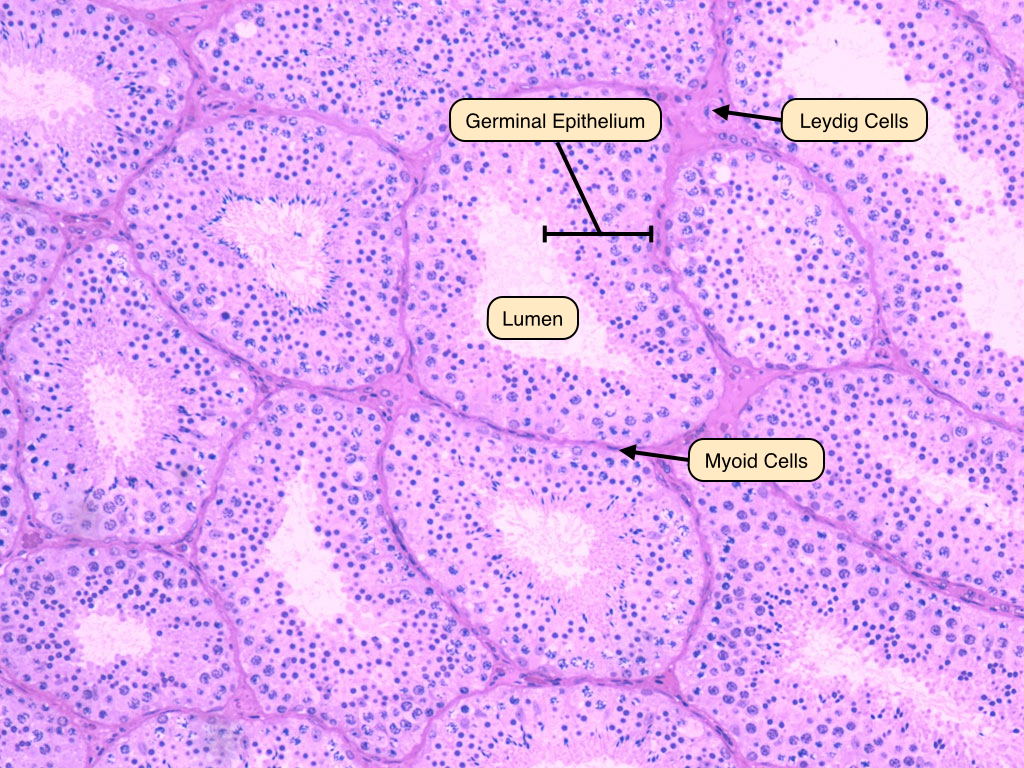
Spermatogenesis
This is magnified image of the germinal epithelium. The epithelium rests on a basement membrane and surrounds a lumen where sprematozoa are released. Identify the spermatogonia, located in the basal compartments of both membranes. These cells appear round and pale, with prominent nucleoli. Sertoli cells, with their characteristic oval-shaped nuclei, are also visible. These provide support to the developing primary spermatocytes, which have large, granulated nuclei that are preparing for the first meiotic division. Secondary spermatocytes, which contain 23 pairs of chromatids, are rarely visible. The products of meiosis are the haploid spermatids, which contain dark, round nuclei and a decreasing amount of cytoplasm. These differentiate further into spermatozoa. Remember that cytokinesis is incomplete during these steps, and cytoplasmic bridges connect the cells and allow for their synchronous development. 
Leydig Cells
Interstitial or Leydig cells are located in the connective tissue surrounding the seminiferous tubules. They produce testosterone, the male sex hormone responsible for the growth and maintenance of the cells of the germinal epithelium and the development of secondary sex characteristics. Leydig cells often display cytoplasmic crystals of Reinke, the function of these crystals is unknown. 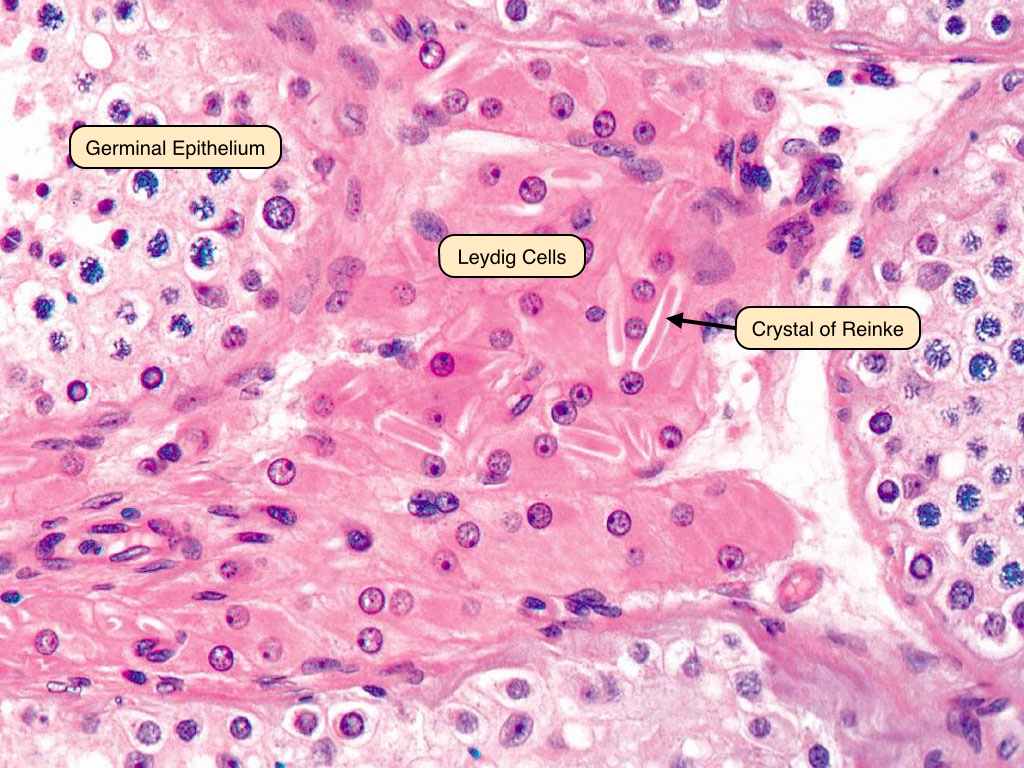
Sertoli Cells
Sertoli cells are located in the germinal epithelium and play a supportive role in the development of spermatozoa. These cells have abundant cytoplasm and extend from the basement membrane to the lumen. Sertoli cells have a characteristic oval nucleus with a dark nucleolus. The cytoplasmic contents and blood-testis barrier are better visualized under the electron microscope. 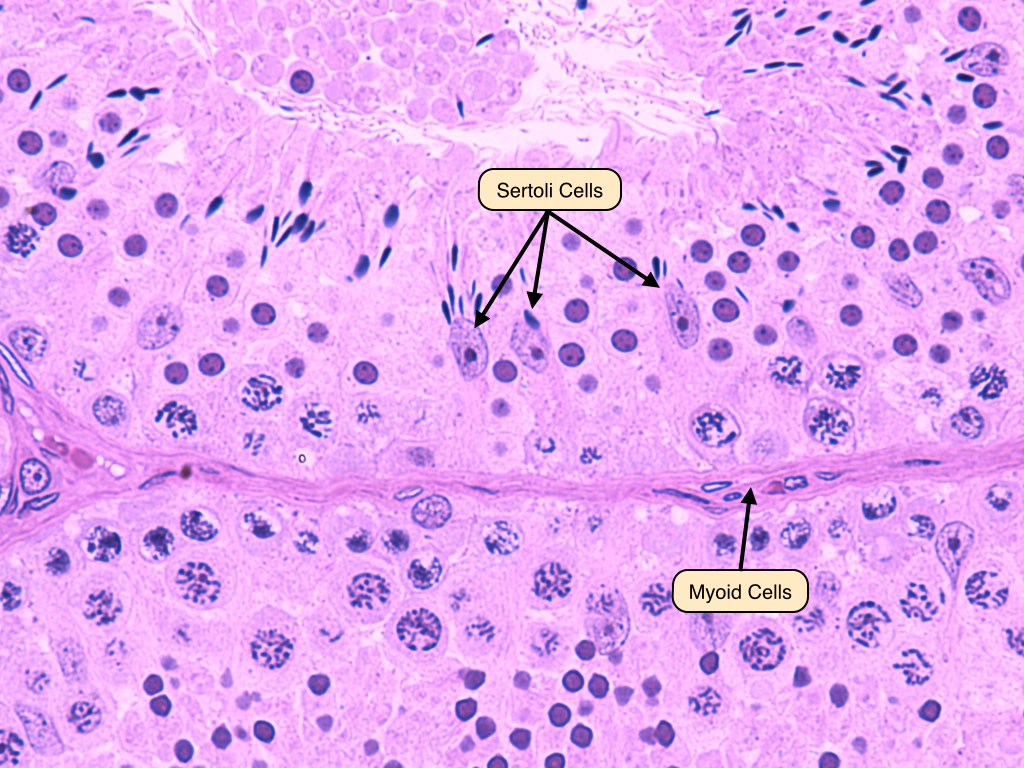
Rete Testis
The rete testis connects the seminiferous tubules to the ductus efferentes. It is lined by ciliated cuboidal epithelial cells that also contain microvilli. The activity of the cilia helps to move the spermatozoa along the tube, as they are immobile until they reach the epididymis. The microvilli absorb excess materials, including protein and potassium, from the seminal fluid. 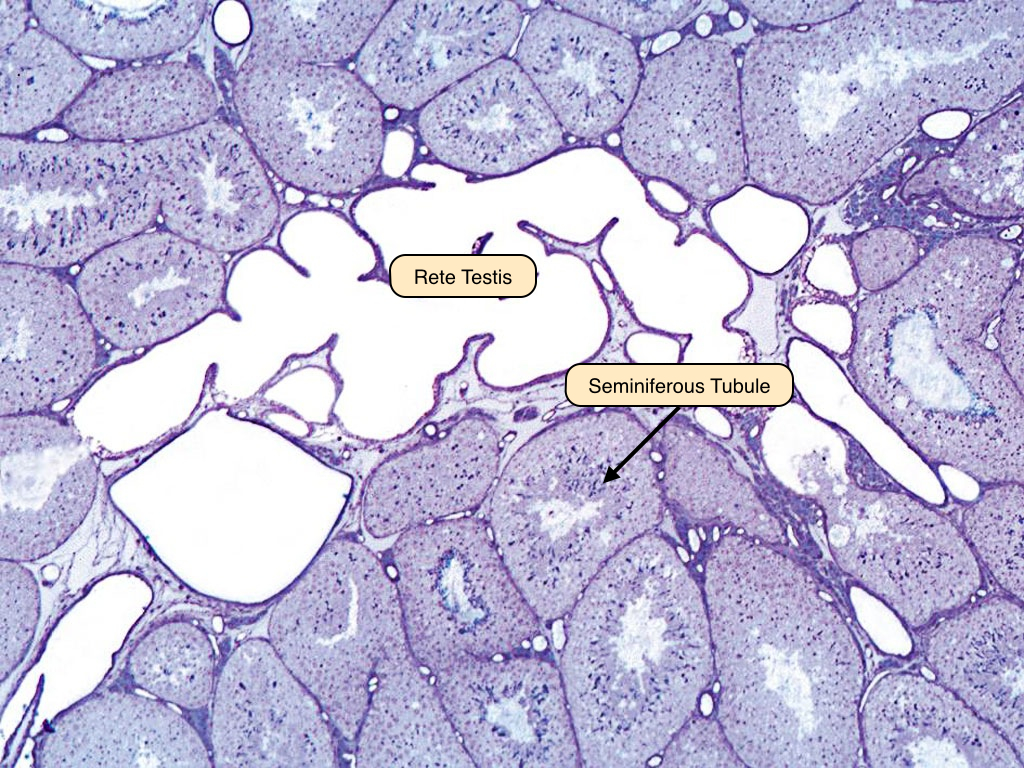
Ductuli Efferentes
The ductuli efferentes emerge from the dorso-superior margin of each testis. They originate from the rete testis and gradually fuse to form the ductus epididymis. The epithelium has a characteristic scalloped appearance that results from a lining that contains both cuboidal and columnar epithelial cells. A layer of smooth muscle surrounds the walls. The non-ciliated cells reabsorb testicular fluid, while the ciliated cells propel the immobile sperm to the epididymis, where they gain the ability to swim. 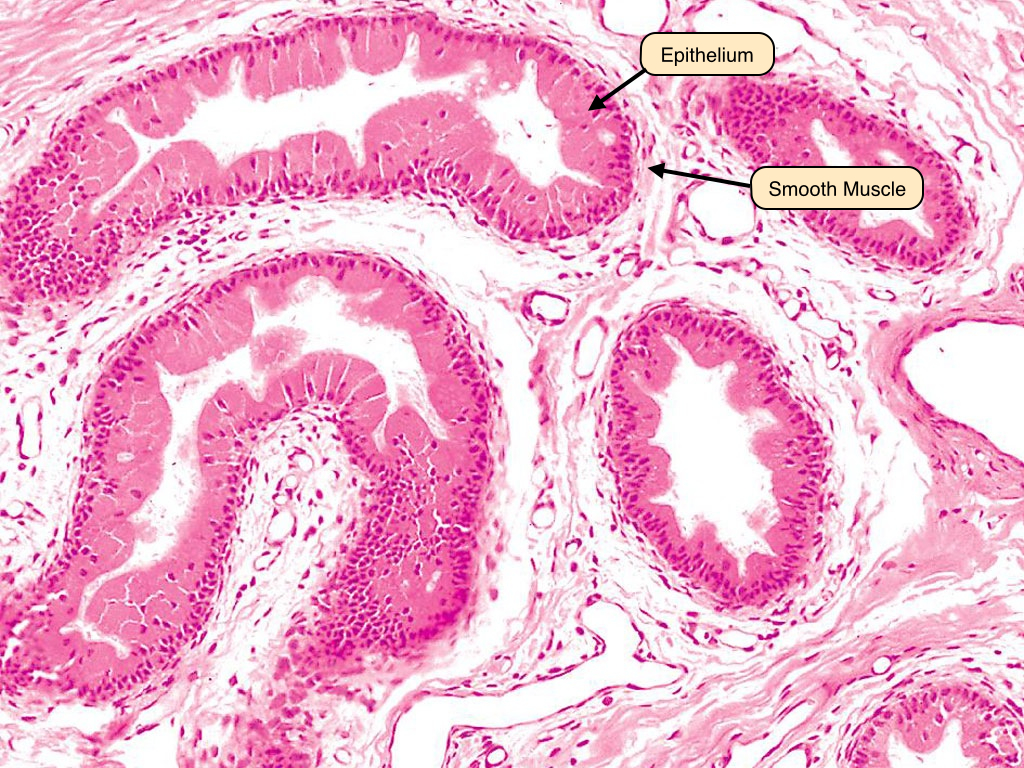
Epididymis
Each epididymis is formed by a single convoluted tubule seen in multiple cross sections. It is lined by a tall pseudostratified columnar epithelium. These cells bear stereocilia on their luminal surface that absorb fluid released from the testes along with sperm. In this section, the spermatozoa can be seen in the lumen throughout the epididymis. 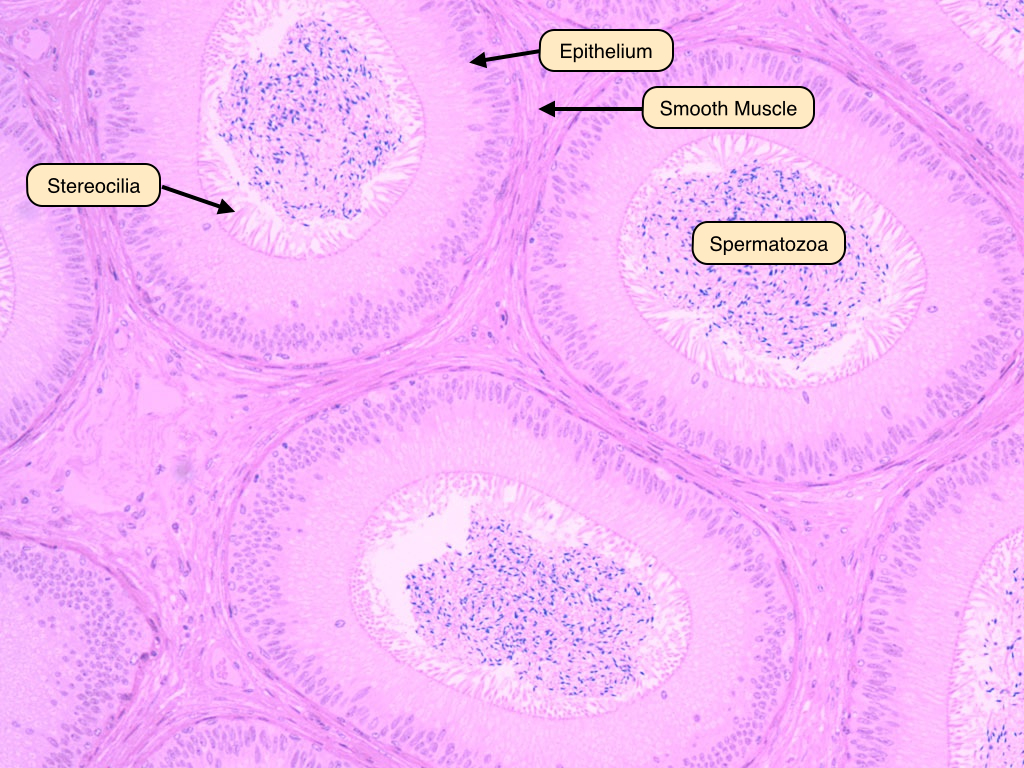
Ductus Deferens
The ductus deferens extends from the epididymis to the ejaculatory ducts. The epithelium of this tube displays a pseudostratified columnar epithelium and is surrounded by a prominent muscular layer. This layer contains inner and outer longitudinal muscle and middle circular muscle. An adventitia of connective tissue surrounds the muscularis layer. 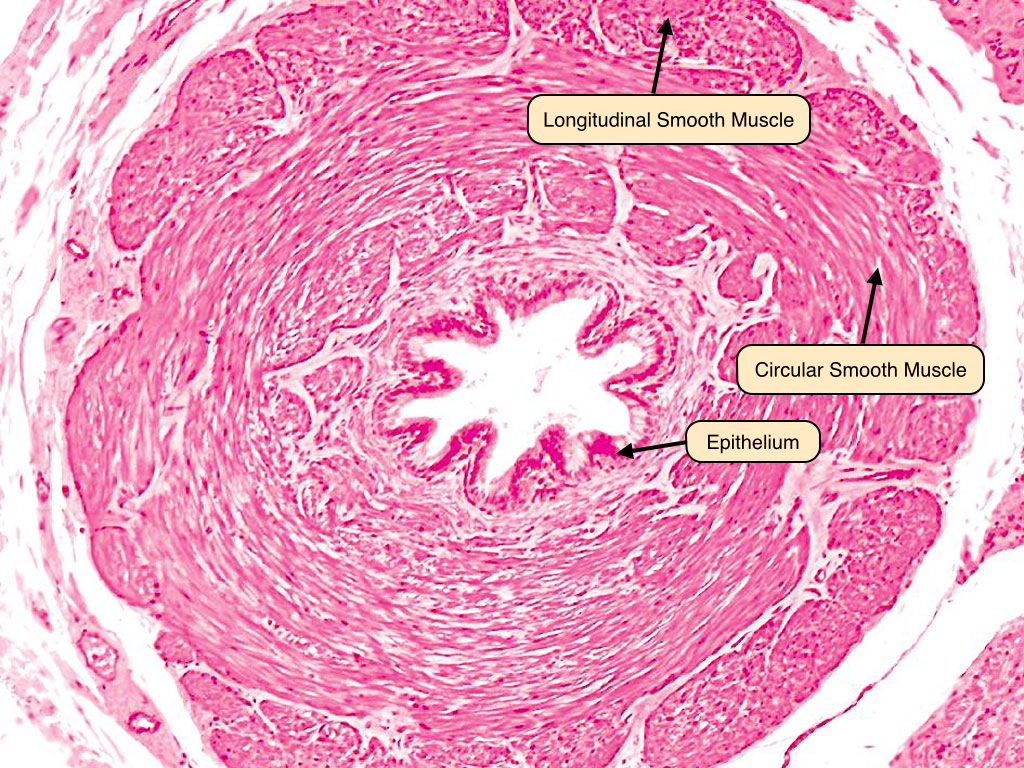
Urethra
The human urethra is lined by a pseudostratified columnar epithelium lining the urethral lumen. The urethra is located in the corpus spongiosum made up of erectile tissue. Note the blood vessels contained in the erectile tissue; during erection, the arteries dilate to fill the sinuses, which obstruct venous outflow and traps blood in the penis. 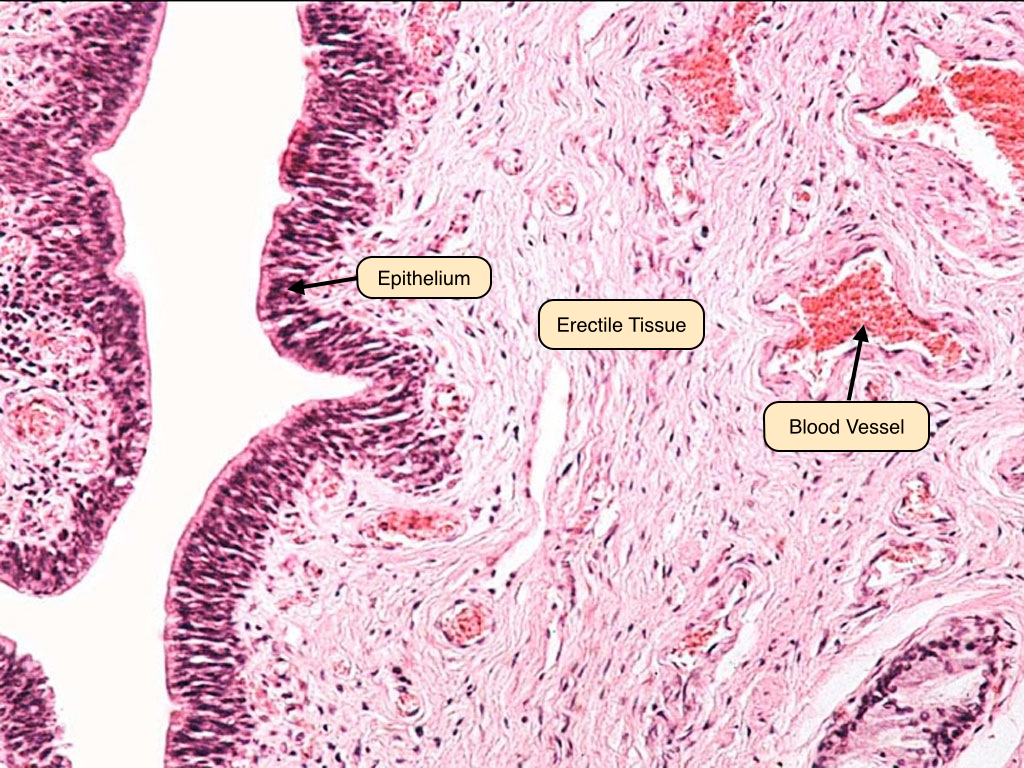
Seminal Vesicle
The seminal vesicles appear as honeycombed saccules with thin, highly branched folds of mucosa, lined by a pseudostratified columnar epithelium. These folds join one another to delimit irregular spaces, which communicate with a large, central lumen filled with a pale-staining, homogenous secretion. Observe the coat of smooth muscle surrounding the saccular dilation of the gland. Its contraction expels the accumulated secretion during ejaculation. 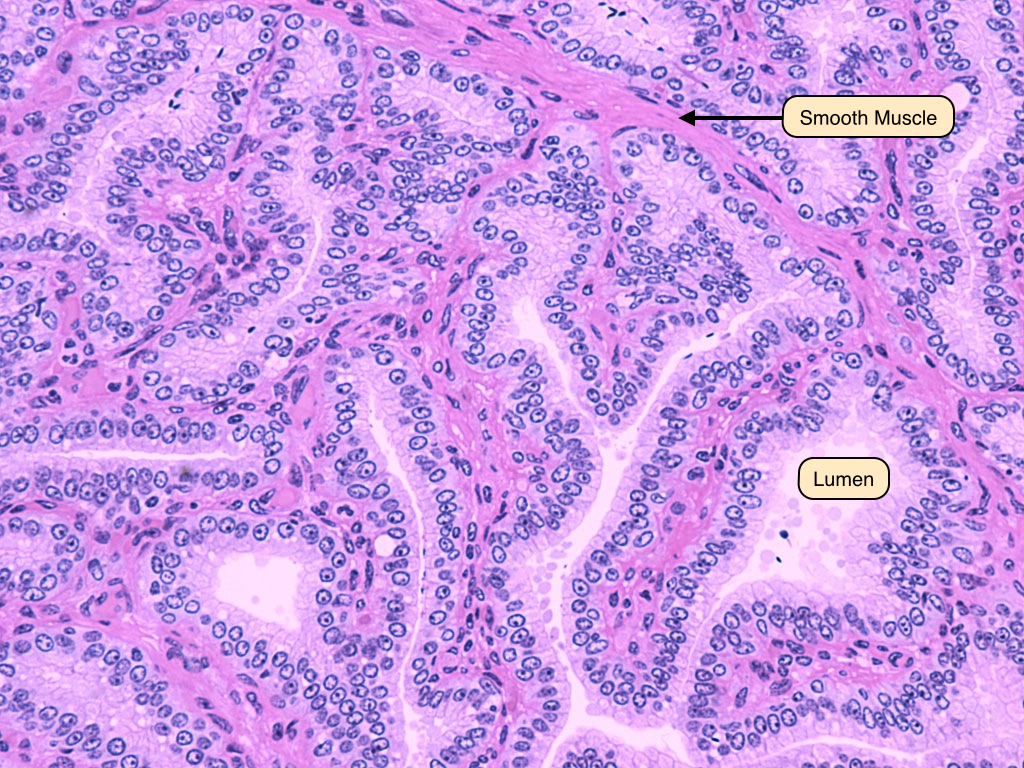
Prostate Gland
The prostate is a walnut-sized conglomeration of tubulo-acinar glands that surrounds the initial segment of the urethra. The epithelium of the prostate produces a fluid rich in citric acid and proteolytic enzymes that nourish and prevent the coagulation of sperm in the vagina. Characteristic of the gland are prostatic concretions. These accumulate over time in the lumina of the tubulo-alveolar glands. Note the presence of numerous basal cells in the epithelium of the glands. Their presence distinguishes benign and malignant glands. 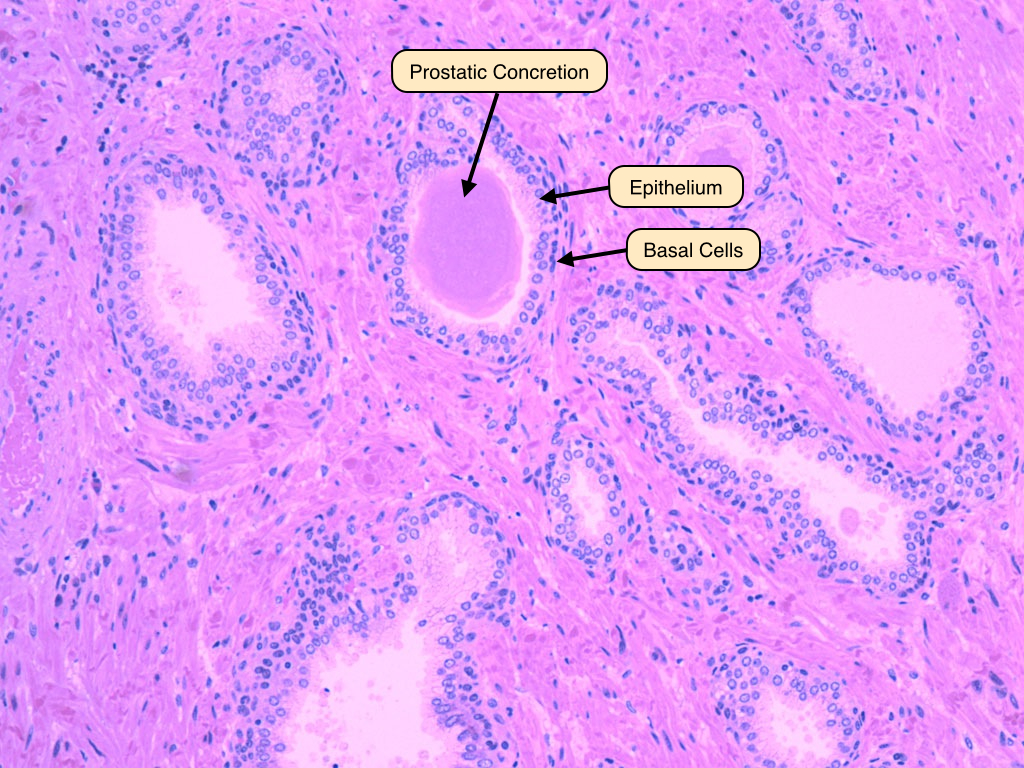
Penis
The penis contains three columns of erectile tissue: two corpus cavernosa and a single corpus spongiosum containing the penile urethra. The erectile tissue of the penis appears as a vast sponge-like system of irregular vascular spaces intercalated between the arteries and veins. These sinuses receive blood from the helicine arteries, which dilate during erection to engorge the sinuses with blood. This, in turn, restricts venous outflow.Note the vast sponge-like arrangement of irregular vascular spaces intercalated between the arteries and veins. 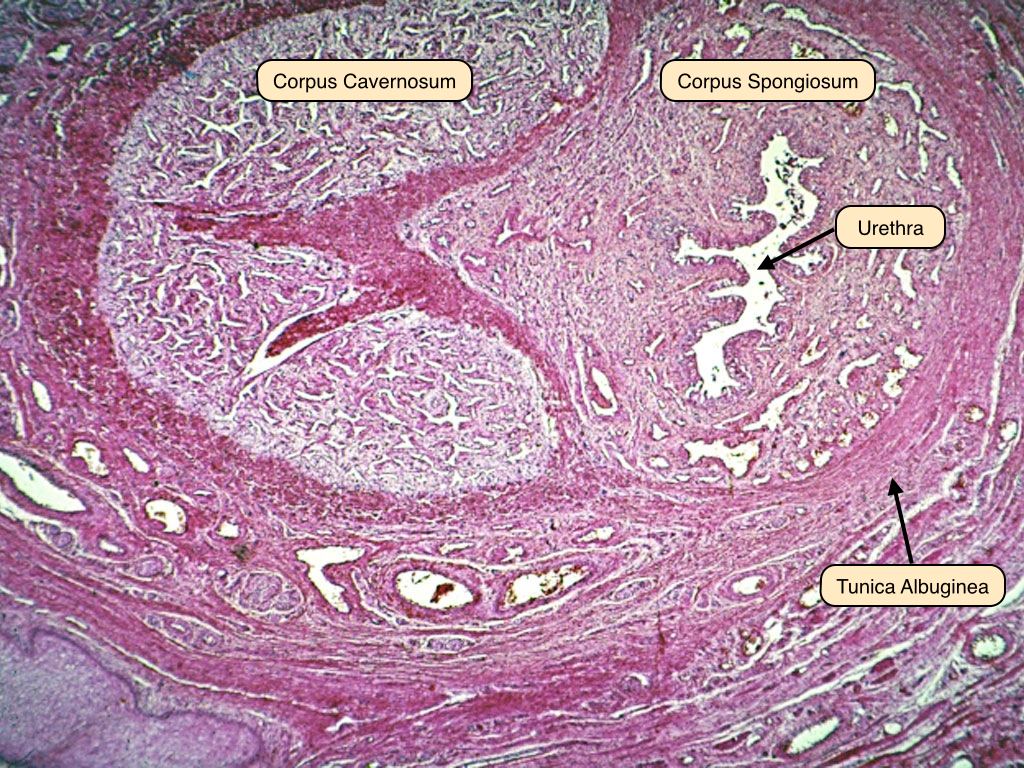
week 6 Endocrine System Histology
Endocrine System Histology
Endocrine Systems Lab
Learning Objectives
- Describe the organization and function of endocrine tissues, including the key endocrine organs as well as diffuse endocrine cells.
- Distinguish the different types of pituitary cells using the light microscope and electron microscope.
- Name and describe the different layers of the adrenal gland, as well as the blood supply to this gland.
- Contrast the structure of the thyroid with that of the parathyroid.
- Identify islets of Langerhans within pancreatic tissue and explain the relative positions of alpha and beta cells.
Lab Content
Introduction
The term "endocrine" implies secretion into the internal milieu of a multicellular organism. In contrast to exocrine tissues, where the secretory products are discharged into the external space - the outer surface of the body, mucosal surfaces, duct systems - the endocrine organs and cells secrete their products into the vascular system. The blood vessels then serve as conduits for these secretions to travel to their target tissues.
Endocrine tissues function according to a basic model. Individual cell types respond, via surface receptors, to different signals. They produce a very limited spectrum of secretory products, called hormones, that themselves function as signaling molecules for specific cell populations. These hormones are effective at exceedingly low concentrations. Because of this, relatively few cells are sufficient for the integrative function of large, multicellular organisms. Therefore, endocrine tissues are characteristically present in small quantities.
Pituitary Gland
The pituitary gland, or hypophysis, is a collection of different cell types that control the activity of other endocrine organs. It is governed by the hypothalamus, which sends both electrical and hormonal signals to the pituitary, and by feedback regulation (both positive and negative) through the secretions of its target glands. This slide shows a section of the human pituitary. In the anterior pituitary (pars distalis), you can see cords of cuboidal cells with a wide range of nuclear to cytoplasmic volume ratios. The posterior pituitary (pars nervosa) is connected to the hypothalamus by the pituitary stalk - this is easily visualized because the nervous tissue appears continuous between the two glands. 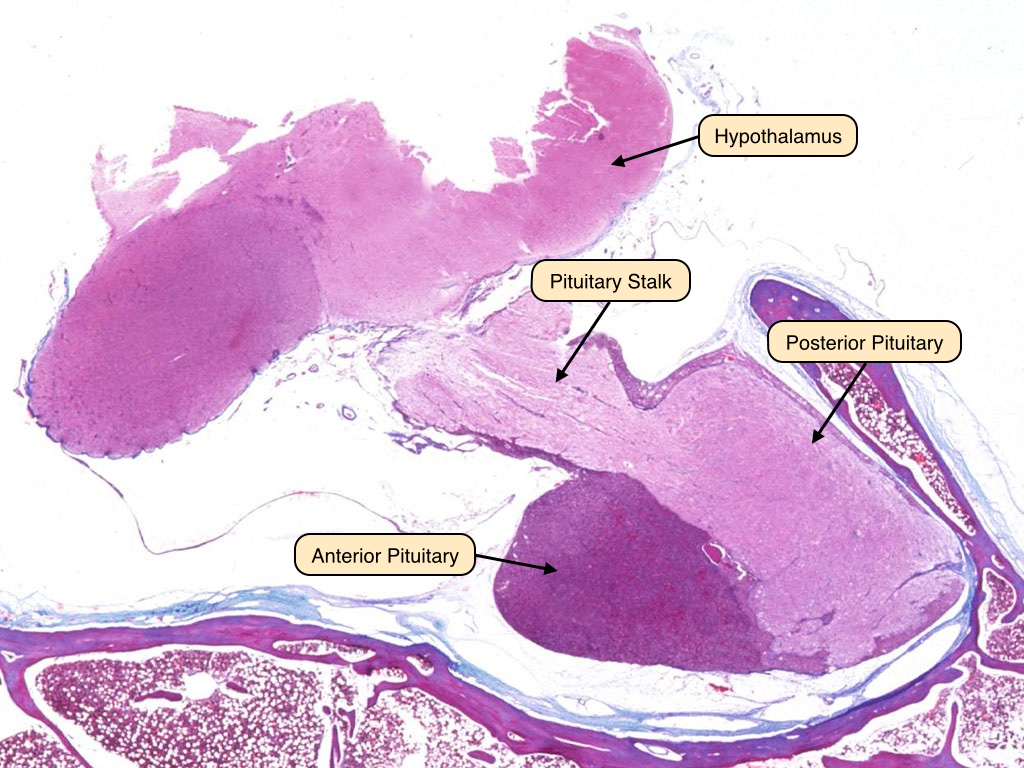
Anterior Pituitary
The anterior pituitary contains cells that, when viewed under the light microscope, appear as acidophils, basophils, or chromophobes. This slide displays the three cell types of the anterior pituitary under H&E stain. The acidophils appear as cells with pink cytoplasm and dark nuclei. These cells secrete protein hormones like growth hormone and prolactin. The basophils appear as darker cells with purple cytoplasm. These cells secrete glycoprotein hormones such as adrenocorticotropic hormone (ACTH), thyroid-stimulating hormone (TSH), follicle-stimulating hormone (FSH), and leutenizing hormone (LH). Finally, a few chromophobes are visible in this section; these cells are non-secretory and serve as support cells or precursors to the acidophils and basophils. 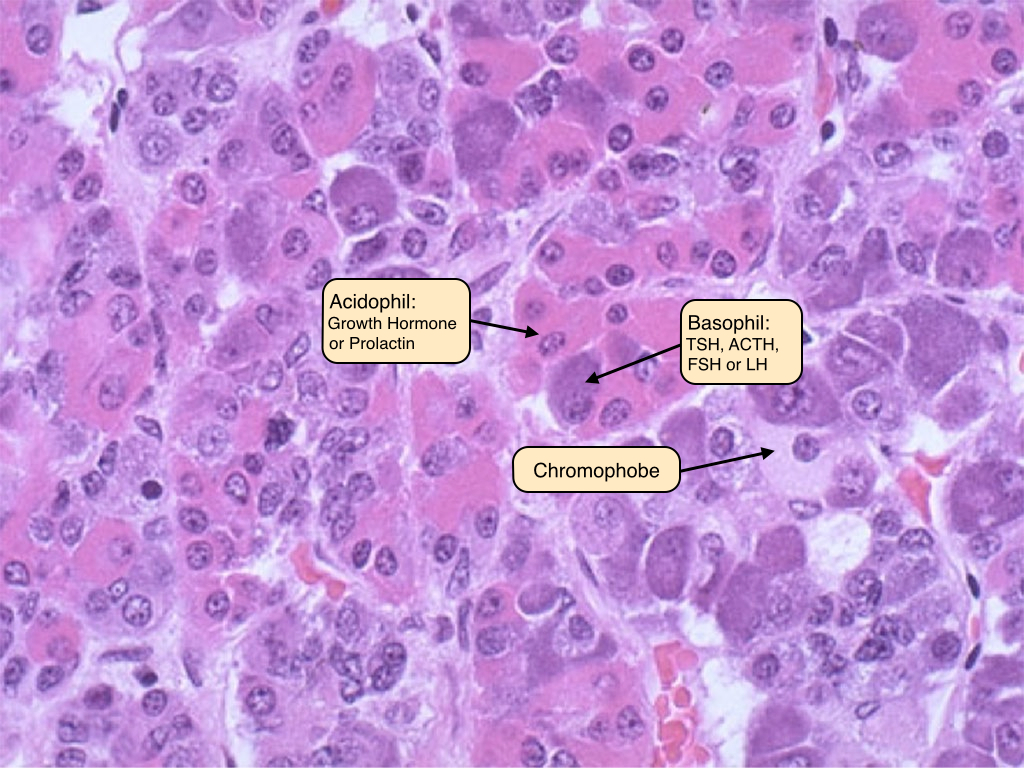
Posterior Pituitary
The posterior pituitary is mostly composed of unmyelinated axonal processes and terminals of the supraoptic and paraventricular nuclei of the hypothalamus. The pituitary stalk connects the two glands. The posterior pituitary has characteristic Herring bodies, focal axonal swellings that are packed with secretory granules. Pituicytes are the glial cells of the pituitary gland; the nuclei that are visible in sections of posterior pituitary belong to these cells, as well as cells of the vasculature. A third section of the pituitary, the intermediate lobe, is vestigial in man. 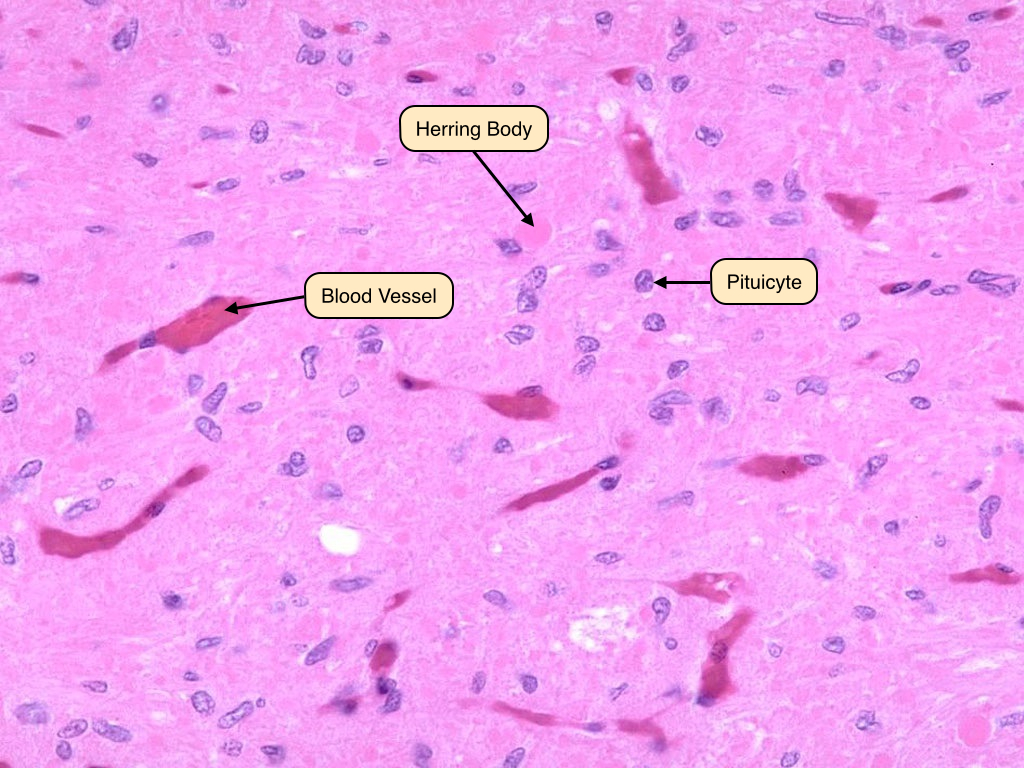
Adrenal Gland
The adrenal gland has two distinct parts, the cortex and medulla, which differ in structure and function. The cortex secretes hormones produced from cholesterol and can be functionally and histologically divided into three zones: glomerulosa, fasciculata, and reticularis. The adrenal medulla is the innermost portion of the gland and shares an embryological origin with the sympathetic nervous system.
The zona glomerulosa is the thin outer layer of the adrenal cortex. Its cells are pale staining and organized in ovoid clusters that are separated by capillaries. The cells of the zona glomerulosa produce mineralocorticoid hormones like aldosterone, which regulates salt and water balance.
The zona fasciculata comprises the thick middle layer of the cortex. Its cells are extensively vacuolated because of the presence of lipid droplets. The cells of this region produce glucocorticoids like cortisol, which has metabolic effects.
The zona reticularis is the innermost layer of the adrenal cortex. The border between it and the zona fasciculata is less distinct than that between the previous two zones. Cells in the zona reticularis stain deeply and are less vacuolated. This region produces androgens, which supplement sex hormones produced by the gonads.
The medulla primarily secretes catecholamines, including adrenaline and noradrenaline. Its cells possess abundant cytoplasmic granules that contain stored peptide hormones and catecholamines. These cells are frequently called chromaffin cells because they can be stained with chromium salts. Preganglionic sympathetic fibers traverse the adrenal cortex and synapse directly on chromaffin cells, where they release acetylcholine to stimulate the exocytosis of catecholamine granules during a sympathetic response. 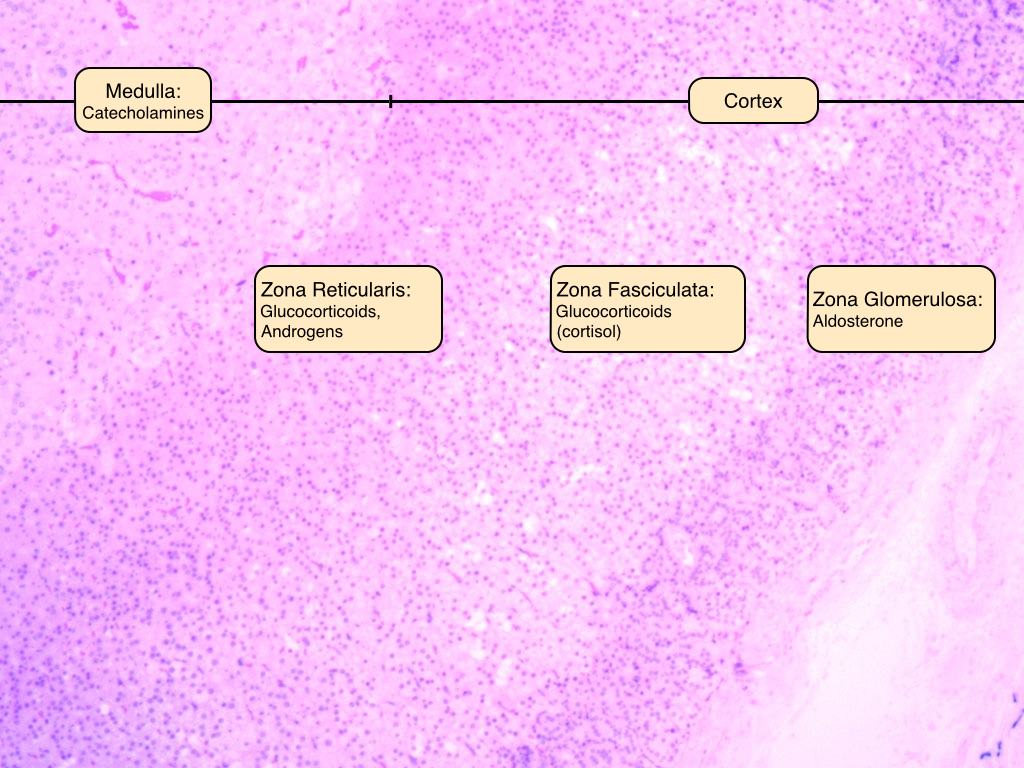
Thyroid
The thyroid is located in the neck and stores large amounts of inactive hormone within extracellular compartments. The thyroid consists of structural units called follicles, which are composed of secretory epithelial cells called principal cells that are adjoined by junctional complexes and surrounded by a basement membrane. Follicles vary in size, but each displays a central lumen containing colloid. Colloid consists of the glycoprotein thyroglobulin, which is secreted by the principal cells and serves as a precursor to thyroid hormone. The height of the principal cells varies according to their level of secretory activity; in hypothyroidism, the cells are squamous or cuboidal, whereas in hyperthyroidism, they are columnar.
Also visible in this slide are a few C-cells, or parafollicular cells, scattered in the spaces between follicles. C-cells secrete calcitonin, which serves as a fine control for calcium homeostasis. 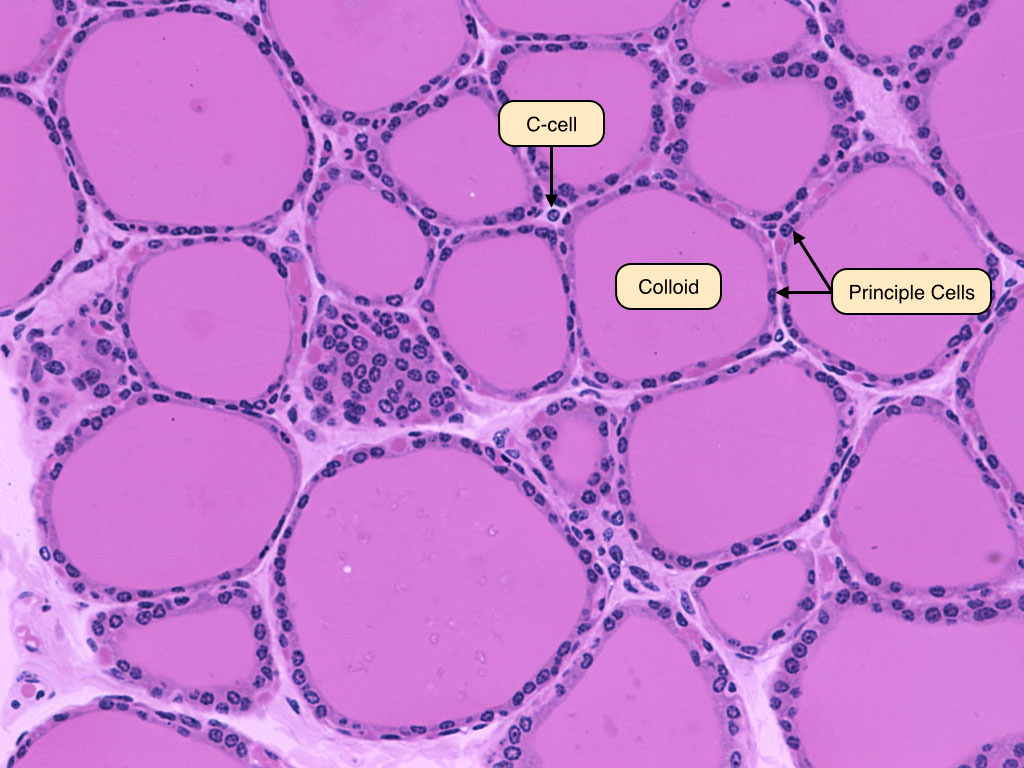
Parathyroid
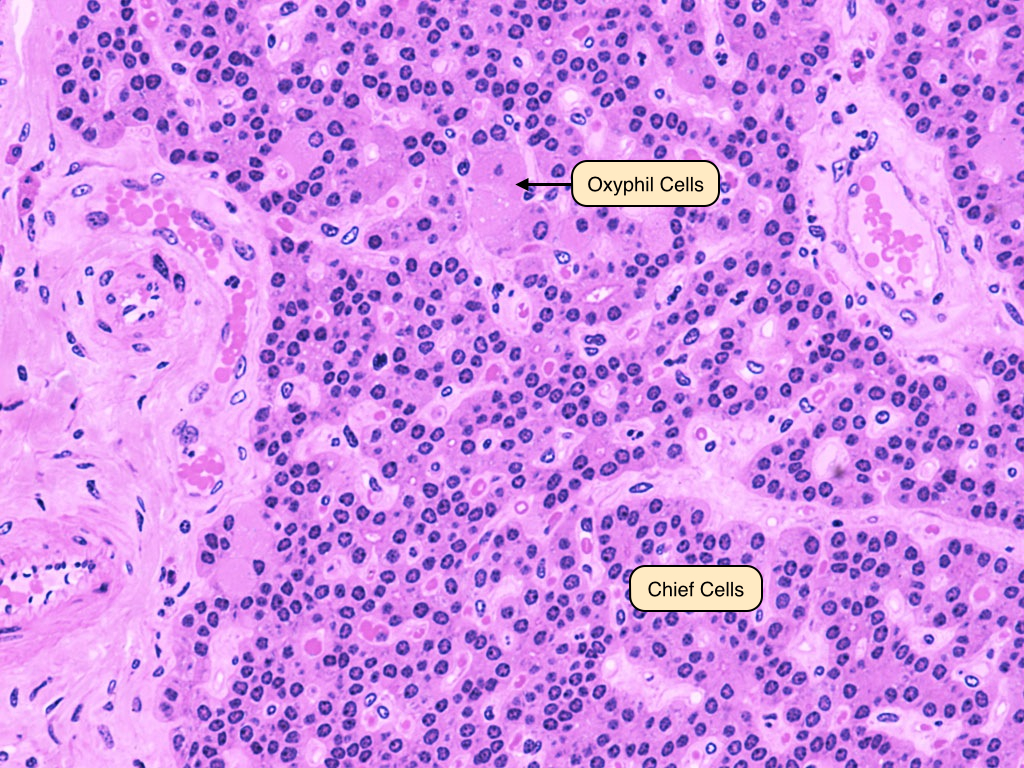
The parathyroid glands are closely associated with the thyroid. They consist of closely packed groups of two cell types:
- Chief (principal) cells, which have prominent central nuclei surrounded by pale cytoplasm. Chief cells produce parathyroid hormone (PTH), which is the most important regulator of calcium metabolism in humans.
- Oxyphilic cells, which are large and fewer in number, have small, dark nuclei and an acidophilic cytoplasm with many mitochondria. The function of these cells is unknown, but they increase in abundance as a person ages.
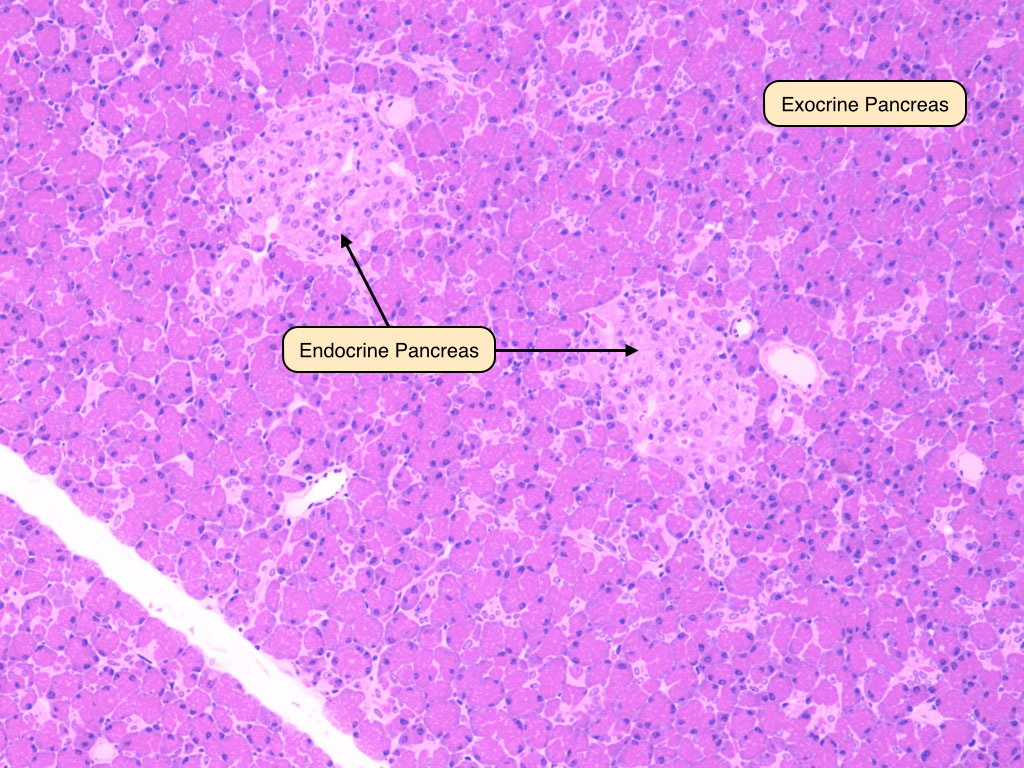
Endocrine Pancreas
The endocrine portion of the pancreas is comprised of the islets of Langerhans. During development, the cells of the islets migrate away from the duct system and aggregate around capillaries. The islets contain three important cell types:
- Alpha cells produce glucagon, which increases the plasma glucose concentration. They are primarily located around the periphery of the islets.
- Beta cells produce insulin, which decreases plasma glucose by promoting uptake by liver, skeletal muscle, and adipose tissue. Beta cells are typically located in the center of the islets.
- D-cells produce somatostain, which has broad effects on gastrointestinal function and inhibits insulin and glucagon secretion. Delta cells are scattered throughout the islets.
week 6The Endocrine System Overview
The Endocrine System Overview
Introduction
The endocrine system is a collection of endocrine glands and cells that act as a control and communication system for the body. The main job of the endocrine system is to maintain homeostasis, which is a stable state of internal conditions optimal for survival. Endocrine organs do this by secreting chemicals called hormones directly into the bloodstream, which carries them to target organs or cells to initiate biochemical and physiological changes.
The primary endocrine organs in the body include the hypothalamus, pituitary gland, pineal gland, thyroid gland, parathyroid glands, thymus, pancreas, thymus, as well as the ovaries in females and the testes in males.
Hypothalamus
The hypothalamus is a structure found in the diencephalon of the brain and is considered part of the endocrine system and nervous system. The main role of the hypothalamus is to control all other endocrine glands. The hypothalamus does this by secreting hormones that regulate the release of other hormones in various endocrine glands. In addition, the hypothalamus is anatomically and functionally linked to the pituitary gland, which hangs from a thin stalk just below it. The hypothalamus-pituitary complex takes stimuli from the nervous system and translates them into hormones which initiate the specific response. The hypothalamus secretes two main types of hormones: releasing hormones such as growth-hormone-releasing hormone (GHRH), which stimulate the secretion of pituitary hormones, and inhibiting hormones such as growth-hormone-inhibiting hormone (GHIH), which stop the secretion of pituitary hormones.
Hormones | Main Effect |
Corticotropin-releasing hormone (CRH) | Stimulates anterior pituitary (AP) to release adrenocorticotropic hormone (ACTH) |
Gonadotropin-releasing hormone (GnRH) | Stimulates AP to release follicle stimulating hormone (FSH) and luteinizing hormone (LH) |
Growth-hormone-releasing hormone (GHRH) | Stimulates anterior pituitary to release growth hormone |
Growth-hormone-inhibiting hormone (GHIH) | Stops anterior pituitary from releasing growth hormone (GH) |
Prolactin-releasing hormone (PRH) | Stimulates anterior pituitary to release prolactin |
Prolactin-inhibiting hormone (PIH) | Stops anterior pituitary from releasing prolactin |
Thyrotropin-releasing hormone (TRH) | Stimulates anterior pituitary to release thyroid-stimulating hormone (TSH) and prolactin |
Pituitary Gland
The pituitary gland is a bean-shaped organ connected to the hypothalamus by a thin stalk called the infundibulum. It forms part of the hypothalamus-pituitary complex that controls numerous other endocrine glands, which is why the pituitary is often called the master gland. The pituitary gland consists of two lobes: an anterior lobe called the adenohypophysis and a posterior lobe called the neurohypophysis. The neurohypophysis secretes a class of hormones called neurohormones that includes oxytocin, which are produced in the hypothalamus but stored in the posterior pituitary. The adenohypophysis secretes a class of hormones called tropic hormones or tropins that includes human growth hormone (HGH), which control the release of other hormones.
Posterior Pituitary Hormones | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
neurohormones | A group of hormones produced by neurosecretory cells in the hypothalamus | ||
antidiuretic hormone (ADH) | Stimulates kidneys to retain water and constrict blood vessels | SIADH | diabetes insipidus |
oxytocin | Stimulates uterine contractions in labor; letdown of milk during breastfeeding | benign prostatic hyperplasia in males | difficult labor; insufficient lactation |
Anterior Pituitary Hormones | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
tropic hormones / tropins | A group of hormones that control the release of other hormones in the body | ||
adrenocorticotropic hormone (ACTH) | Stimulates production of cortisol by adrenal glands | Cushing’s syndrome | Addison’s disease |
follicle stimulating hormone (FSH) | Regulates reproductive processes such as puberty and gonad function | enlarged ovaries in females | lack of sexual development; infertility |
human growth hormone (HGH) | Stimulates body growth and development | gigantism; acromegaly | pituitary dwarfism |
luteinizing hormone (LH) | Regulates gonad function and the menstrual cycle in females | decreased sex steroid production by gonads | lack of sexual development; infertility |
melanocyte-stimulating hormone (MSH) | Stimulates the production of the pigment melanin in melanocytes | skin darkening | skin lightening |
prolactin | Stimulates milk production and breast development in females | excessive lactation | insufficient lactation |
thyroid-stimulating hormone (TSH) | Stimulates thyroid gland and regulates thyroid function | hypothyroidism, Hashimoto’s thyroiditis | hyperthyroidism; Grave’s disease |
Anterior Pituitary
Posterior Pituitary
Pineal Gland
The pineal gland is a small, cone-shaped gland located between the two lobes of the thalamus in the brain. The main role of the pineal gland is to regulate the body’s circadian rhythm or sleep-wake cycle. The pineal gland does this by releasing the hormone melatonin. Melatonin levels vary with the amount of light in the environment. When light levels are rise, less melatonin is released, promoting wakefulness. When light levels fall, more melatonin is released, causing sleepiness.
Hormone | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
Melatonin | Regulates body’s circadian rhythm; regulates secretion of other hormones | seasonal affective disorder (SAD) | sleep problems; mood disorders |
Thyroid Gland
The thyroid is a butterfly-shaped gland located in the throat just below the larynx. The thyroid wraps around the front and sides of the trachea and consists of two lateral lobes connected by a band of tissue called an ismus. The main role of the thyroid is to regulate body metabolism and to reduce blood calcium levels. The thyroid does this by releasing three hormones: triiodothyronine (T3), thyroxine (T4), and calcitonin. Triiodothyronine and thyroxine increase the metabolism of body cells and calcitonin stimulates bone cells to absorb more calcium from the blood, thus decreasing blood calcium levels.
Hormones | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
calcitonin | Stimulates absorption of calcium by bones; lowers blood calcium levels | hypocalcemia | hypercalcemia |
triiodothyronine (T3) | Stimulates body metabolism; more powerful than thyroxine (T4) | hyperthyroidism; Grave’s disease | hypothyroidism, Hashimoto’s thyroiditis |
thyroxine (T4) | Stimulates body metabolism; less powerful than triiodothyronine (T3) |
Parathyroid Glands
The parathyroid consists of four rice-shaped glands embedded in the posterior surface of the thyroid, two glands per lobe. The main role of the parathyroid is to increase blood calcium levels. The parathyroid does this by releasing parathyroid hormone (PTH). PTH stimulates bone cells to release calcium into the blood and causes the kidneys to increase calcium reabsorption. These two effects act to increase blood calcium levels. In this way, parathyroid hormone acts in opposition (antagonistically) to the hormone calcitonin that is released by the thyroid.
Hormone | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
parathyroid hormone (PTH) | Stimulates release of calcium by bones; increases blood calcium levels | hypercalcemia | hypocalcemia |
Thymus
The thymus is a triangular gland located directly under the sternum in the chest area between the lungs. The main role of the thymus is to stimulate the development and maturation of T-cells which function in the body’s immune system. To do this, the thymus releases thymosin. The thymus is relatively large in children and continues to grow until puberty. In adults, the thymus slowly decreases in size and is eventually replaced by fatty tissue.
Hormone | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
Thymosin | Stimulates development of mature T-cells for the immune system | Myasthenia gravis | Reduced immunity |
Pancreas
The pancreas is a long, flat organ located just below the stomach that belongs to both the endocrine system and digestive system. The digestive functions of the pancreas include releasing digestive enzymes into the gastrointestinal tract. The endocrine functions of the pancreas include releasing hormones which regulate blood glucose levels. The functional unit of the pancreas are clusters of glandular cells called the islets of Langerhans, which come in two types. Alpha cells release the hormone glucagon, which stimulates the liver to release glucose into bloodstream, thus increasing blood glucose levels. Beta cells release the hormone insulin, which stimulates body cells to absorb glucose from the bloodstream, thus decreasing blood glucose levels.
Hormones | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
glucagon (beta cells) | Stimulates liver to release glucose into blood; increases blood glucose levels | hyperglycemia; diabetes (Type 1) | - |
insulin (alpha cells) | Stimulates body cells to absorb glucose; decreases blood glucose levels | hypoglycemia; insulin shock | hyperglycemia; diabetes (Type 1) |
Adrenal Glands
The adrenal glands are two cone-shaped organs located on top of each kidney.
There are two major layers of each adrenal gland: an inner layer called the adrenal medulla, and an outer layer called the adrenal cortex.
The main role of the adrenal medulla is to help stimulate the body’s “fight or flight” response to stress. To do this, the medulla releases a class of hormones called catecholamines that includes epinephrine and norepinephrine. Epinephrine and norepinephrine complement the action of the sympathetic nervous system and prepare the body for greater physical performance.
The main role of the adrenal cortex is to help regulate the body’s mineral balance, energy balance, and reproductive functions. To do this, the cortex releases three classes of hormones. The first class of hormones are called glucocorticoids and include cortisol. Cortisol regulates blood glucose levels and acts as an anti-inflammatory compound. The second class of hormones are called mineralocorticoids and include aldosterone. Aldosterone regulates the concentration of electrolytes in the blood, especially sodium and potassium, which in turn affects blood volume and blood pressure. The adrenal cortex also releases a small amount of steroid sex hormones, including androgens, estrogen, and progestin. Sex hormones influence the development of secondary sexual characteristics and regulate reproductive system function in both sexes.
Adrenal Medulla Hormones | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
catecholamines | A group of hormones that help the body respond to stress or fright | ||
epinephrine (adrenalin) | Stimulates “fight or flight” response; prepares body for stress | symptoms of stress | - |
norepinephrine (noradrenalin) | |||
Adrenal Cortex Hormones | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
glucocorticoids | A group of hormones involved in metabolizing carbohydrates, proteins, and fats | ||
cortisol (cortisone) | Regulates blood glucose levels; helps metabolize carbohydrates, proteins &fats | Cushing’s syndrome | Addison’s disease |
mineralocorticoids | A group of hormones involved in regulating fluid and electrolyte levels | ||
aldosterone | Regulates electrolyte levels; influences blood pressure and blood volume | water retention | dehydration |
steroid sex hormones | A group of hormones responsible for reproductive and secondary sex characteristics | ||
androgens | Stimulates development of secondary sexual characteristics; regulates reproductive system function | premature sexual development | lack of sexual development |
estrogen | |||
progestin | Promotes conditions needed for pregnancy in females | low blood pressure, swelling | infertility |
The Ovaries
The ovaries are two oval-shaped glands located on either side of the uterus in females. Ovaries are the female gonads and produce mature female sex cells called ova. As endocrine organs, the main role of the ovaries is to produce steroid sex hormones. Sex hormones, which include estrogen and progesterone, regulate the female reproductive system and stimulate secondary sex characteristics such as breast development and menstruation.
Hormone | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
estrogen | Stimulates development of female sex characteristics; regulates reproductive system | premature sexual development | fatigue; loss of sex drive, depression |
progesterone | Regulates female menstrual cycle; prepares and maintains body for pregnancy | adrenal hyperplasia | irregular menstruation; early labor |
The Testes
The testes are two oval-shaped glands located inside the scrotal sac in males. The testes are the male gonads and produce mature male sex cells called sperm or spermatocytes. As endocrine organs, the main role of the testes is to produce steroid sex hormones. Sex hormones, which include testosterone and androgens, regulate the male reproductive system and stimulate secondary sex characteristics such as muscle development and hair growth.
Hormone | Main Effect | Hypersecretion Disorders | Hyposecretion Disorders |
testosterone | Stimulates development of male sex characteristics; regulates reproductive system | premature sexual development | fatigue; loss of sex drive, depression |
androgens |
WHAT ARE HORMONES?
Introduction to the Endocrine System
The endocrine system is a collection of endocrine glands and cells that acts as a control and communication system for the body. The main job of the endocrine system is to maintain homeostasis, which is a stable state of internal conditions optimal for survival.
To achieve homeostasis, endocrine glands secrete hormones, which are chemicals transported by the bloodstream throughout the body that act on target cells to produce a specific response. Hormones regulate numerous body functions (listed below) and come in two types: steroid hormones and nonsteroid or amino acid hormones.
Body Functions Regulated by Hormones | ||||
Metabolism and Energy Balance | Water and Electrolyte Balance | Body Defenses | Growth and Development | Reproduction |
Steroid Hormones
Steroid hormones include cortisol, testosterone, and estrogen.
Steroid hormones are lipid-based since they are derived from a cholesterol precursor and are therefore structurally similar to it. Thus, steroid hormones are complex carbon-ring structures.
Steroid hormones act by the primary messenger pathway. Since they are lipid-based, they can easily diffuse across the cell membrane of their target cell. Once inside, steroid hormones bind with an intracellular receptor in the cytoplasm to form a hormone-receptor complex. The complex passes through the nuclear membrane and binds to the cell’s DNA where it regulates the expression of certain genes. This action causes an increase or decrease in the production of corresponding proteins, such as cellular enzymes, which alters the activity or function of the target cell.
Nonsteroid Hormones
Oxytocin, melatonin, and epinephrine are nonsteroid hormones.
Nonsteroid hormones are not lipid based as they are derived from amino acids. Nonsteroid hormones come in 3 types. Protein hormones, such as insulin, are long chains of amino acids. Peptide hormones, such as oxytocin, are short chains of amino acids. Amine hormones, like melatonin and epinephrine, are a single modified amino acid.
Nonsteroid hormones act by the secondary messenger pathway. Since they are not derived from lipids, they are not fat soluble and cannot diffuse across the cell membranes of their target cell. Nonsteroid hormones bind with an external receptor on the cell membrane of the target cell. This triggers the release of a secondary messenger molecule, which activates cellular enzymes, which alters the activity or function of the target cell.
Feedback Loops
Many body processes are regulated by mechanisms called feedback loops. A feedback loop is a circuit of cause-and-effect where the output of the system is used as input for future changes. In other words, the system “feeds back” into itself. A home thermostat is an example of a feedback loop. The temperature in the home is set by the thermostat and is continually monitored by a sensor inside the unit. When the temperature of the home drops below the point at which the thermostat is set, the thermostat turns on the furnace. As the temperature in the house rises, the thermostat senses the change and turns the furnace off when the temperature reaches the set point. There are two main types of feedback loops in the body: negative feedback loops and positive feedback loops.
-
se cs of fibrosis Fibroblasts Clot formation Macrophages Connected tissue process Wound contraction process Regenerate healing process ...
-
Digestive System Histology GI Tract Learning Objectives Describe the histological characteristics of the layers comprising each segment of...
-
https://ecrcommunity.plos.org/2015/06/05/just-skin-deep-your-immune-system-at-the-surface/

