Lymphatic & Immune System Histology
Lymphatics Lab
Learning Objectives
- Explain the flow of lymph through the lymph node and blood through the spleen, and how the structure of these organs facilitates their function
- Distinguish the between B- and T-cell regions of lymphoid tissue
- Recognize the differences in appearance and function between red and white pulp in the spleen
Lab Content
Introduction
The immune system is important for the elimination of harmful foreign pathogens, which it achieves via its ability to distinguish self from non-self. A broad spectrum of pathology may result when the system is not functioning properly; some of the examples include immunodeficiency, autoimmunity, and hypersensitivity. In addition, the immune system is capable of identifying and eliminating cancer cells, and is thus important in cancer surveillance.
This lab focuses on two organs with roles in facilitating an immune response: lymph nodes and the spleen. Lymph nodes are specialized sites of antigen presentation (between antigen presenting cells and lymphocytes) and lymphocyte activation and proliferation. The spleen is a site of interaction between blood-borne antigens and lymphocytes and another site for lymphocyte activation and proliferation.
Lymph Nodes
Lymph nodes occur along the course of the lymphatic vessels. They filter the lymph as it drains back to the bloodstream. Lymph nodes are important sites of interaction between antigens, antigen presenting cells, and lymphocytes. Normally, they are only a few millimeters in diameter. However, when an immune response is initiated, the lymphocytes within the lymph nodes undergo activation and proliferation, causing the nodes to enlarge.
This is a low power view of a lymph node, which is encased by a capsule. Lymph nodes are usually bean-shaped, with an indented region known as the hilum. They are covered by a collagenous capsule that extends into the body of the node as trabeculae or septa. The body of the lymph node is divided into an outer cortex and an inner medulla. The cortex contains a high concentration of lymphocytes while the inner medulla is less cellular. Note the B-cell containing lymphoid follicles located in the cortex. Between the cortex and medulla lies an ill-defined region called the paracortex which is rich in T-cells. The hilum of the lymph node is the location where blood vessels enter and exit the node. It is also where the medullary sinuses merge into efferent lymphatic vessels, which carry the lymph away from the node. 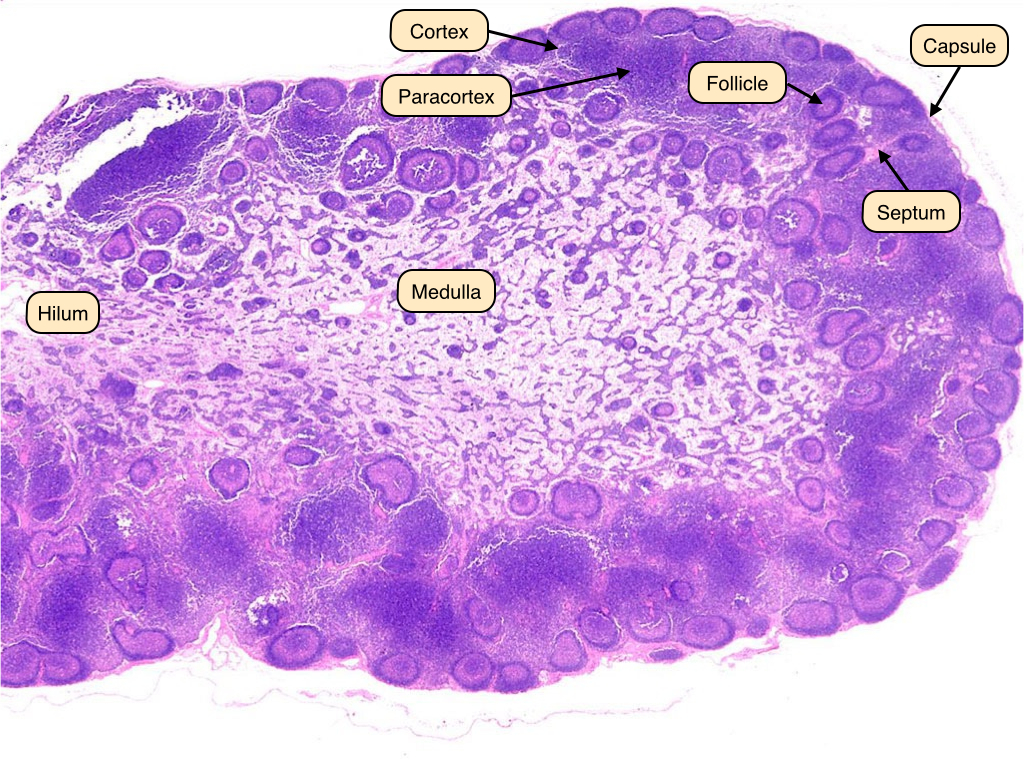
Lymph Node Capsule
This is a high power view of the lymph node capsule and subcapsular sinus. Lymph enters the node via afferent lymphatic vessels, which are located within the capsule. Lymph from the extracellular space carries antigens and antigen presenting cells such as dendritic cells and macrophages from the tissues to the lymph nodes. The lymphatic vessels contain valves, which are clearly seen in this slide. The subcapsular sinus is lined by a layer of endothelial cells. Beneath the endothelial cells are macrophages that retrieve antigen from the lymph in the subcapsular sinus. These macrophages cannot be distinguished in histological images. 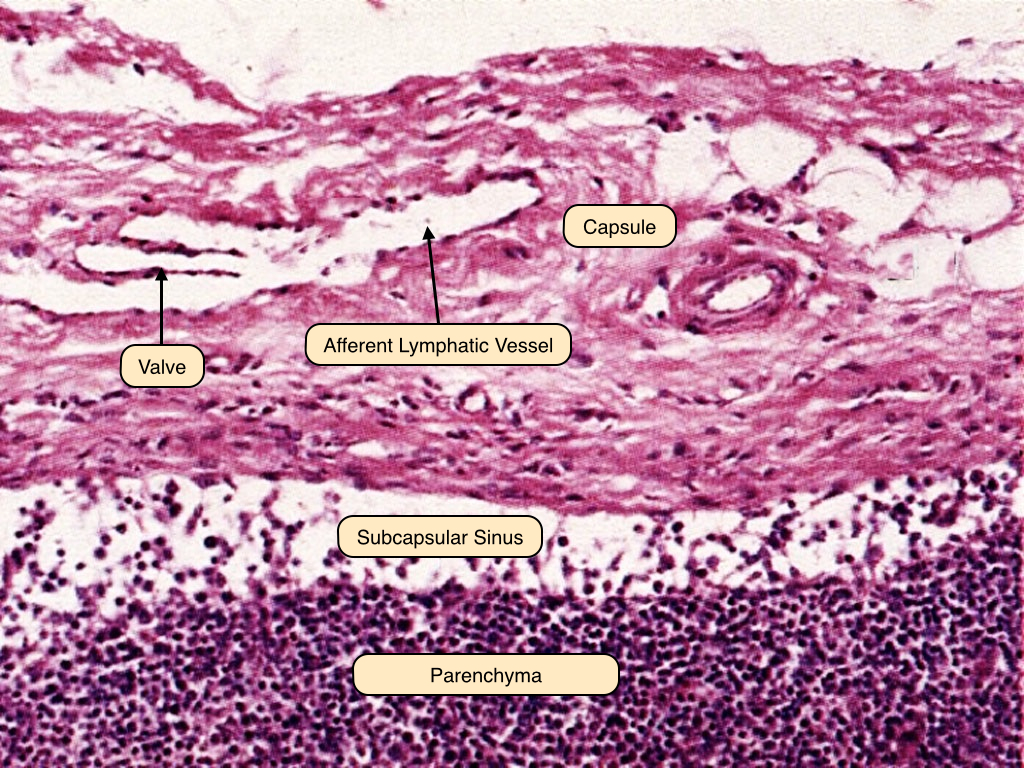
Lymph Node Secondary Follicle
This is a medium power view of a secondary follicle in a lymph node. Note the pale germinal center, which contains proliferating B-cells and follicular dendritic cells. As B-cells proliferate, they undergo somatic hypermutation (mutation of the immunoglobulin gene) in order to enhance the binding affinity between the antigens and the antibodies. The mantle zone of the follicles contains resting and memory B-cells. 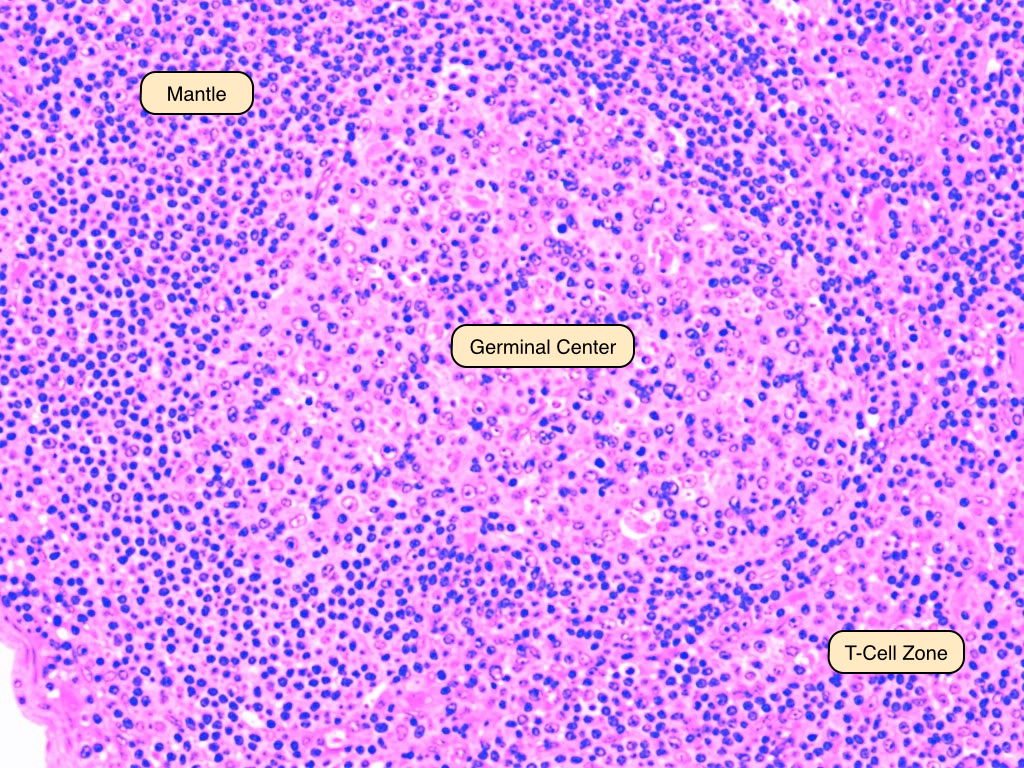
Lymph Node Paracortex
The paracortex of the lymph node is a T-cell zone. One feature of this region is the high endothelial venule, where circulating lymphocytes leave the bloodstream to enter the node. These postcapillary HEVs can be distinguished by their cuboidal endothelial cells. Adhesion molecules called selectins and integrins on the surfaces of HEVs and lymphocytes mediate attachment of lymphocytes to endothelial cells. In a T cell-dominant immunological response, one may observe expansions of the paracortical region. 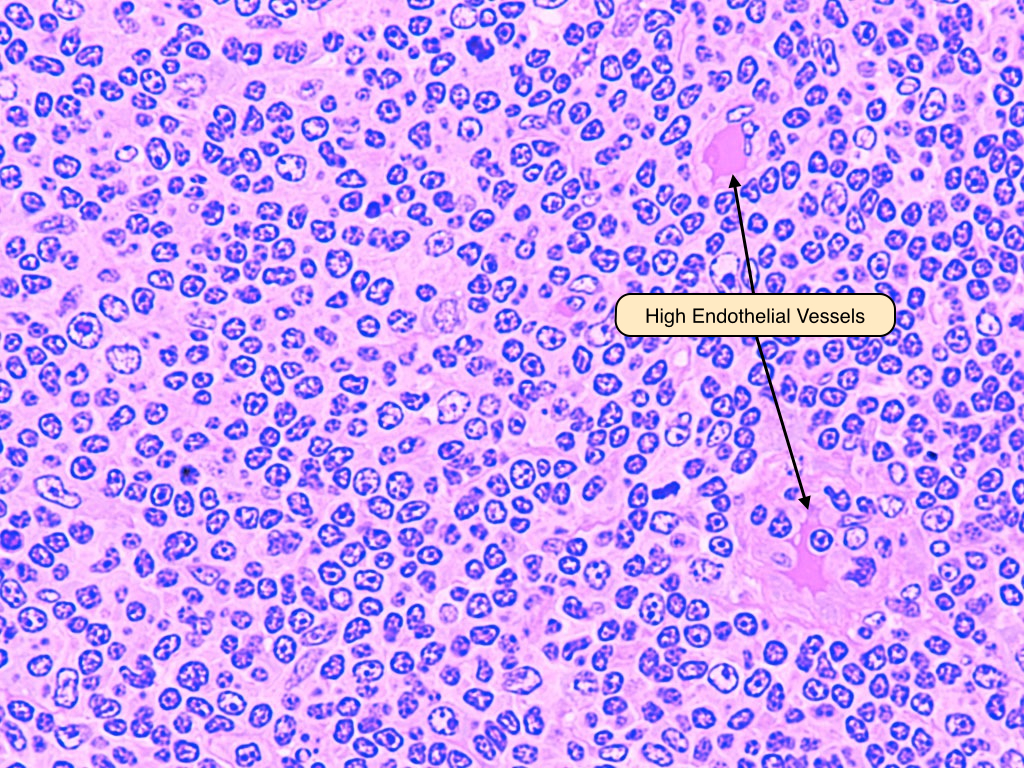
Spleen
The spleen is an organ located in the upper left quadrant of the abdomen. It serves three main functions:
- Activation of immunity against antigens from the blood
- Disposal of senescent blood cells, particularly erythrocytes
- Hemopoiesis in fetus (and in adults with particular diseases)
Like the lymph nodes, the spleen is covered by an outer capsule that extends into the parenchyma as trabeculae. The majority of the spleen is composed of a matrix called the red pulp, which is the site of erythrocyte disposal. Embedded within the red pulp are small white nodules called the white pulp. These nodules contain the lymphocytes. 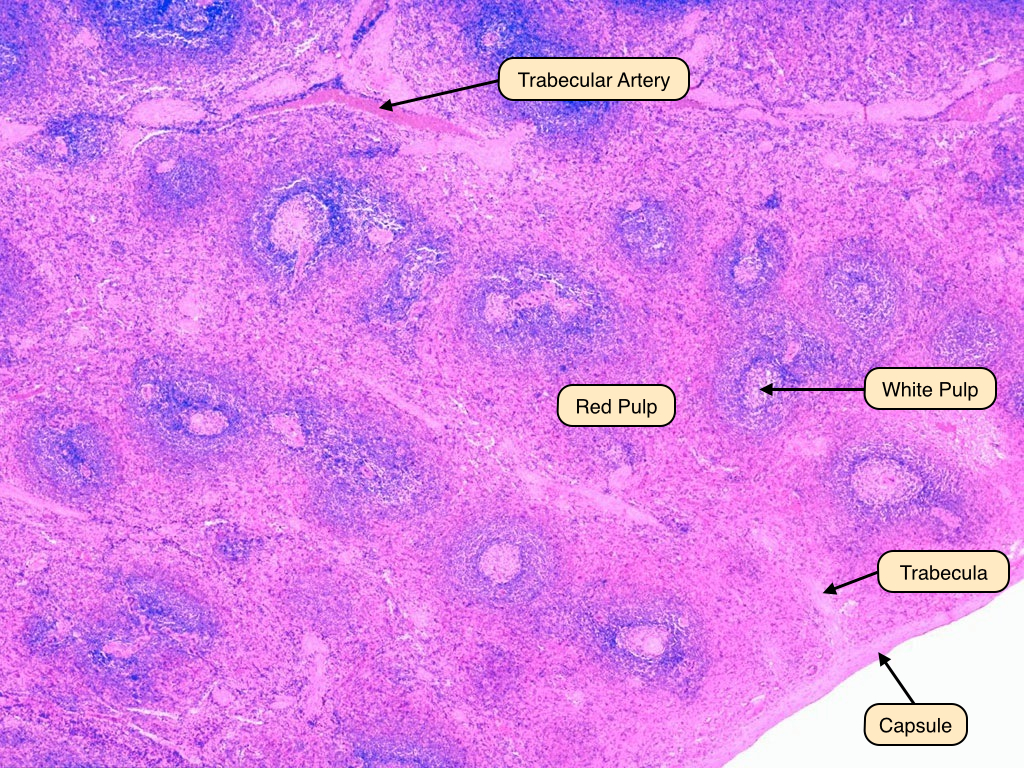
Spleen Central Artery
Central arteries branch from trabecular arteries and run throughout the white pulp. They are surrounded by groups of T-cells that a form a structure called the periarteriolar lymphoid sheath. 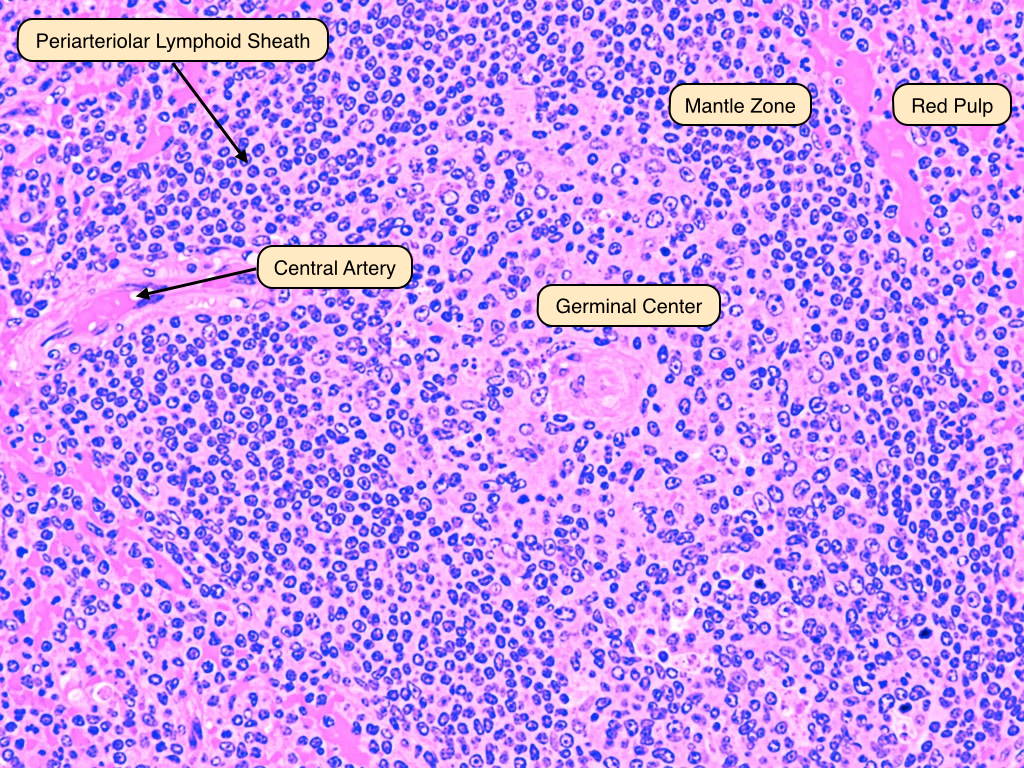
Spleen White Pulp
In the white pulp, the vessel is surrounded by the periarteriolar lymphoid sheath (PALS), which is made up of mostly T-cells. At the border of the PALS lies the follicle, which consists mainly of B-cells. Surrounding the follicle are the narrow mantle zone, which contains packed lymphocytes, and a broader marginal zone, which contains more diffuse lymphocytes. The follicle here is a secondary follicle, as evidenced by the presence of a pale-staining germinal center. The germinal center is surrounded by a narrow ring of deep-stained mantle that contains resting B-cells. The marginal zone separates the follicle from the red pulp. 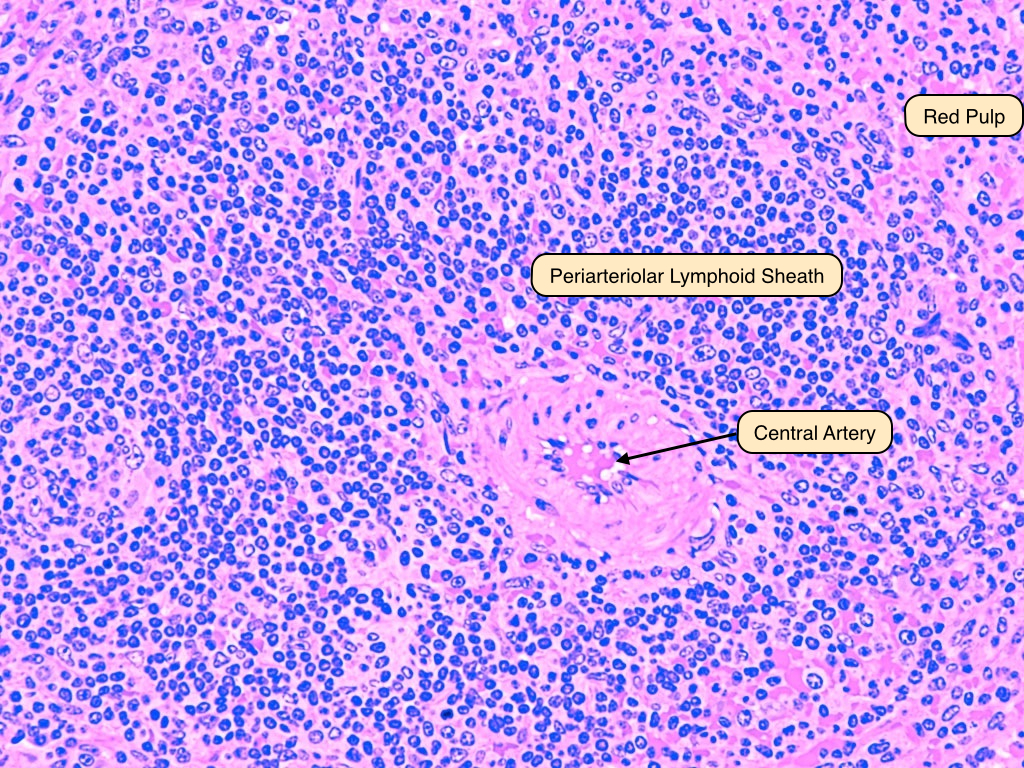
Spleen Red Pulp
The red pulp is mainly filled with venous sinuses, which contain red blood cells and occasionally white blood cells. The sinuses are lined by elongated, rod-shaped endothelial cells. In the sinuses, old or abnormal red cells that have lost their ability to deform are removed by macrophages, while healthy blood cells can squeeze through the walls of the sinuses and are transported out of the organ by the splenic vein. Slits between the endothelial cells allow viable red blood cells to squeeze into the sinuses from the splenic parenchyma. These sinuses eventually drain into the splenic vein. 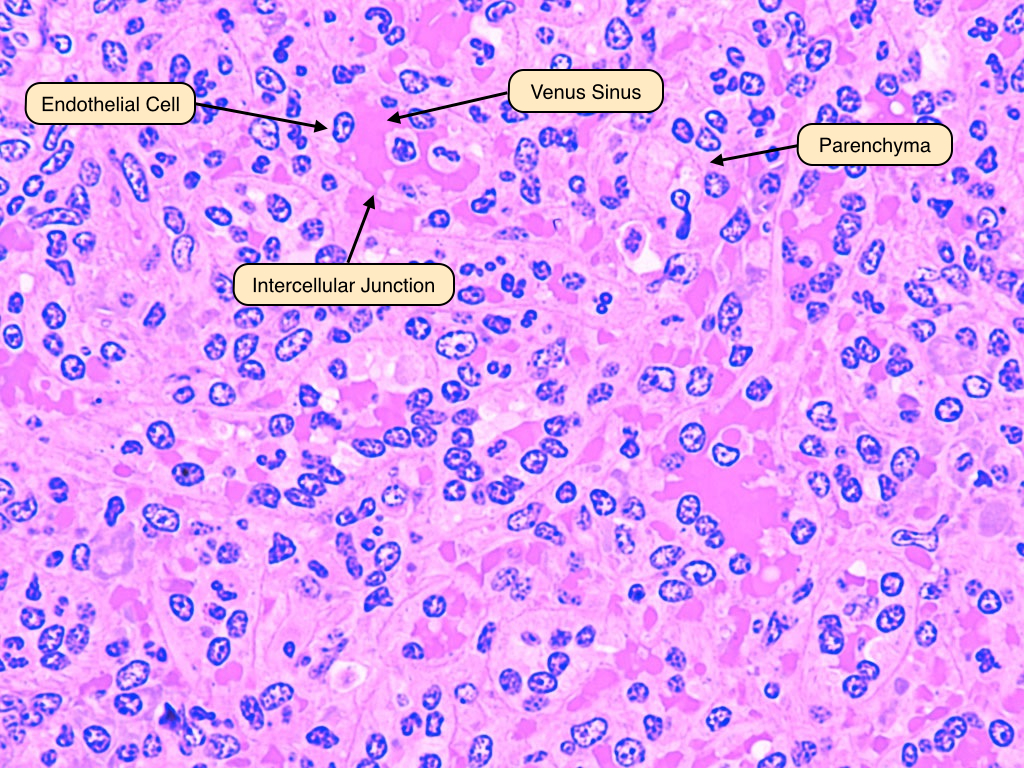


No comments:
Post a Comment