Female Reproductive System Histology
Female Reproductive System Lab
Learning Objectives
- Explain the regular progression of follicular development and atresia occurring in a cyclic fashion in the primary ovary
- Describe the structural changes that occur in the uterus over the course of the menstrual cycle and pregnancy
- Characterize the histological features of the oviduct, uterus, cervix, and vagina, with particular attention to the mucosal linings of these tissues
Pre-Lab Reading
Introduction
The female reproductive system is unique in that its histological appearance cycles and undergoes structural changes that are not pathological. This laboratory will focus on the female reproductive system throughout the course of the menstrual cycle and pregnancy. It is necessary to have a conceptual understanding of the changes that occur in the ovary and uterus during these events so that the histological findings can be understood in the context of reproductive physiology.
Overview of the Female Reproductive System
The female reproductive system is composed of two gonads known as ovaries, two oviducts, the uterus, the vagina and external genitalia, and two mammary glands. Its development, maturation, and functioning is dependent upon a complex interplay of hormones from the hypothalamus, pituitary gland, adrenal glands, ovaries, and placenta.
The system has six primary functions:
- Produce ova via oogenesis
- Receive spermatozoa
- Provide an environment for fertilization
- Provide an environment for fetal development
- Expel the developed fetus
- Provide nutrition to the newborn
Ovary
The human ovary consists of an inner medulla and outer cortex with indistinct boundaries. The medulla contains the blood vessels and nerves, while the cortex is occupied by developing follicles. Visible in this ovary are follicles in various stages of development. Also visible is a corpus luteum, the remnants of a follicle that has burst and sent its ovum into the genital tract. 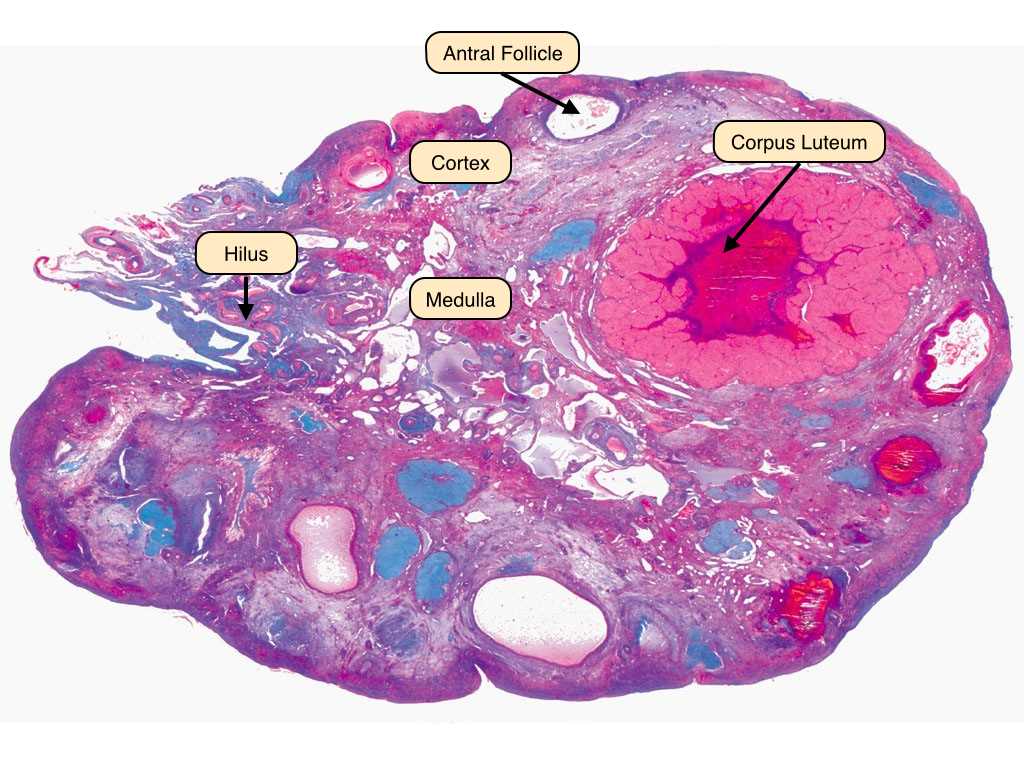
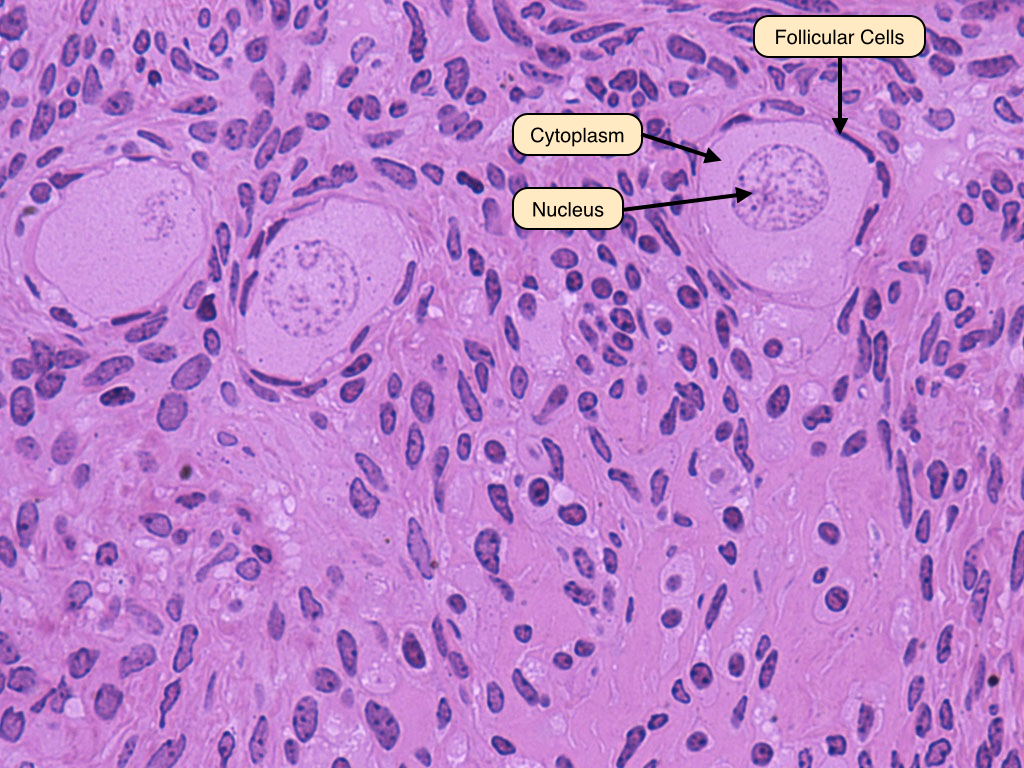
Primordial Follicles
An ovarian follicle progresses through several distinct phases before it releases its ovum. During the first five months of development, a finite number of primordial follicles form in the fetal ovary. These follicles consist of oocytes surrounded by a single layer of squamous follicular cells. These primordial follicles remain in the process of the first meiotic division. At puberty, they begin to develop further and become primary follicles.
Early Primary Follicle
The primary follicle has a central oocyte and is surrounded by a single layer of cuboidal cells. The zona pellucida is a thin band that separates these two layers. 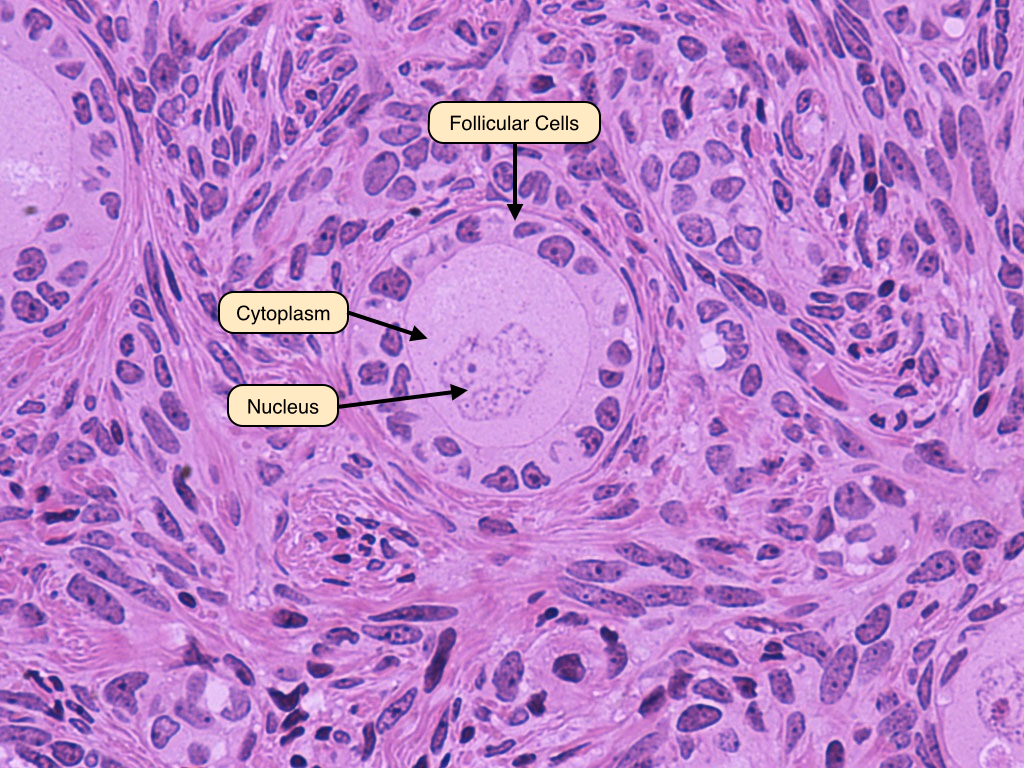
Late Primary Follicle
The late primary follicle stage is achieved when the follicular cells proliferate into a stratified epithelium known as the zona granulosa. The zona pellucida can be seen even more clearly in this image. 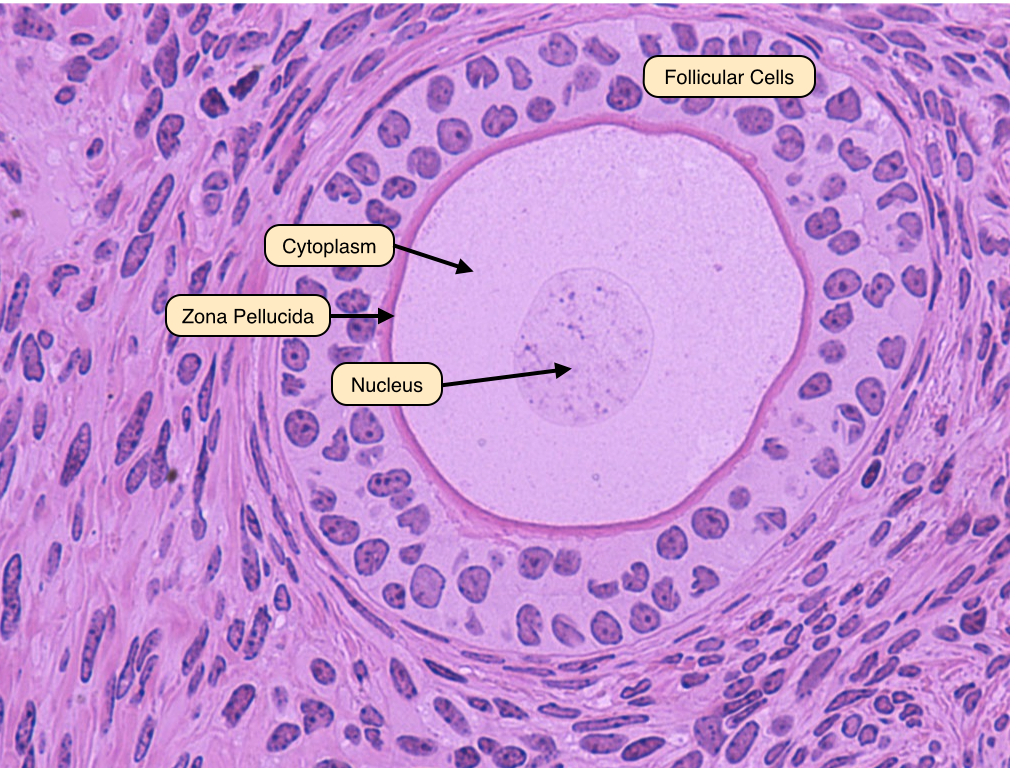
Secondary Follicle
The characteristic feature that distinguishes secondary from primary follicles is the appearance of a follicular antrum within the granulosa layer. This gap contains fluid known as liquor folliculi. Also visible in this image are the oocyte and the zona pellucida. The follicle is surrounded by the theca interna, whose cells produce hormones. 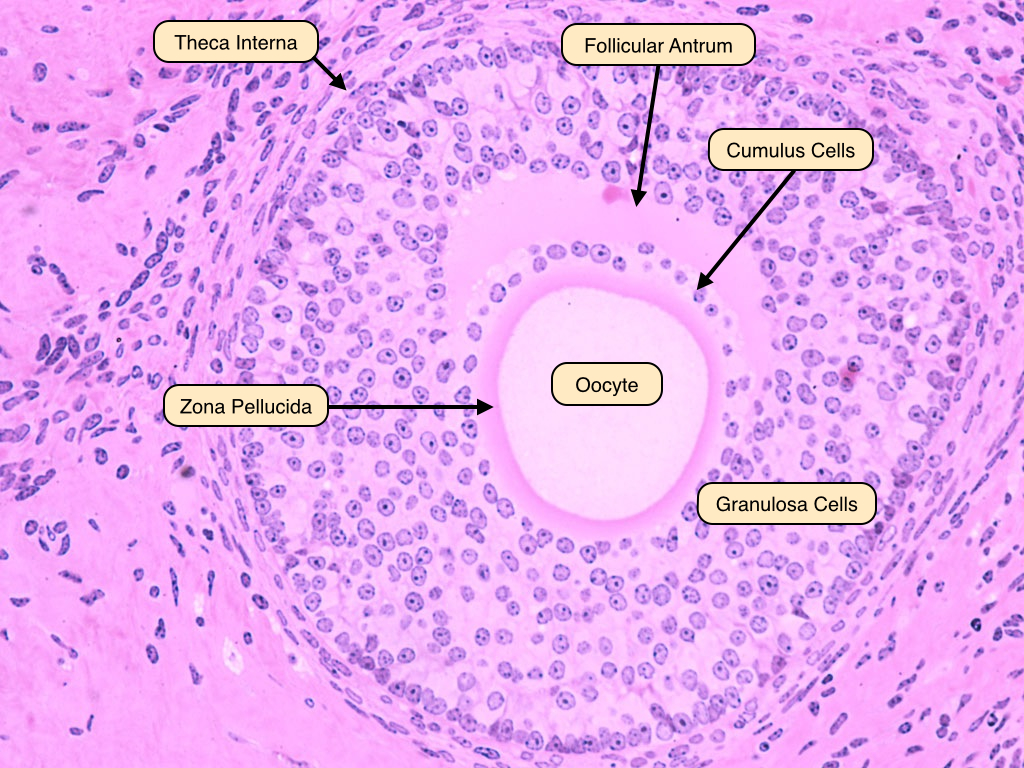
Graafian Follicle
The Graafian follicle is the follicular stage after the first meiotic division but before ovulation. It therefore contains a 2N haploid oocyte. It is characterized by a large follicular antrum that makes up most of the follicle. The secondary oocyte, having undergone the first meiotic division, is located eccentrically. It is surrounded by the zona pellucida and a layer of several cells known as the corona radiata. When released from the Graafian follicle and into the oviduct, the ovum will contain three layers: oocyte, zona pellucida and corona radiata. 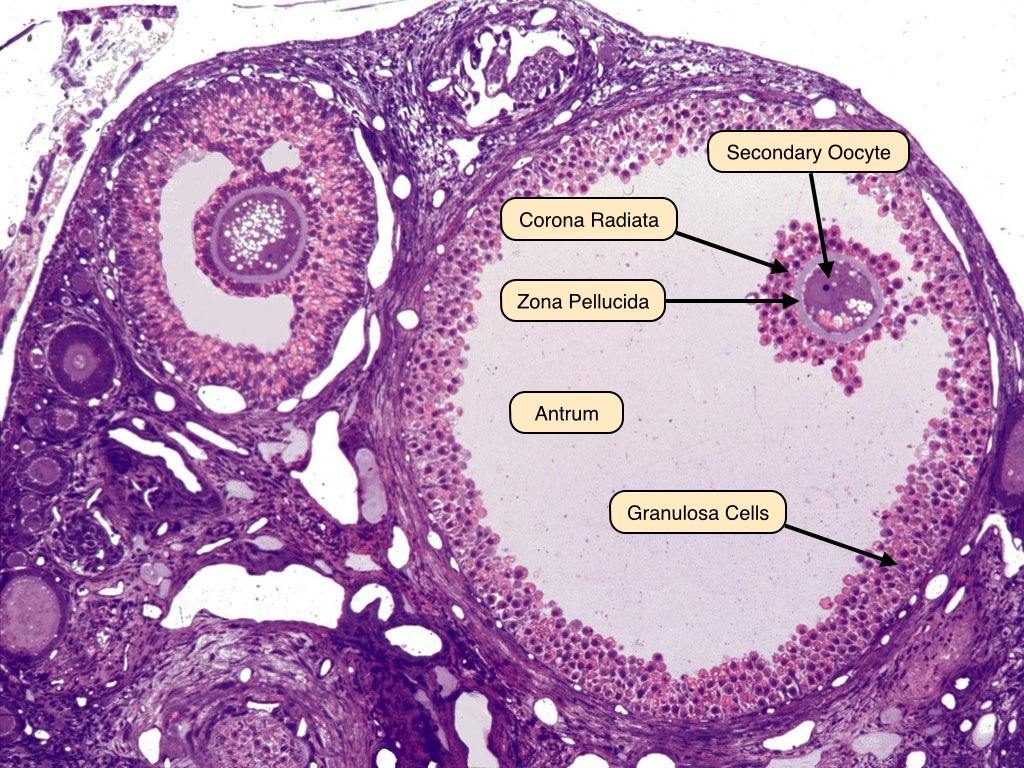
Corpus Luteum
The corpus luteum is the endocrine remains of the collapsed follicle. The center contains the remains of the blood clot that formed after ovulation. Surrounding the clot are glanulosa lutein cells and on the outside theca lutein cells.

Lutein Cells
The granulosa lutein cells have an appearance characteristic of steroid-producing cells, with pale cytoplasm indicating the presence of lipid droplets. Theca lutein cells are smaller and more deeply stained. If fertilization and implantation ensue, the corpus luteum will be maintained by hCG and remain active as the corpus luteum of pregnancy. 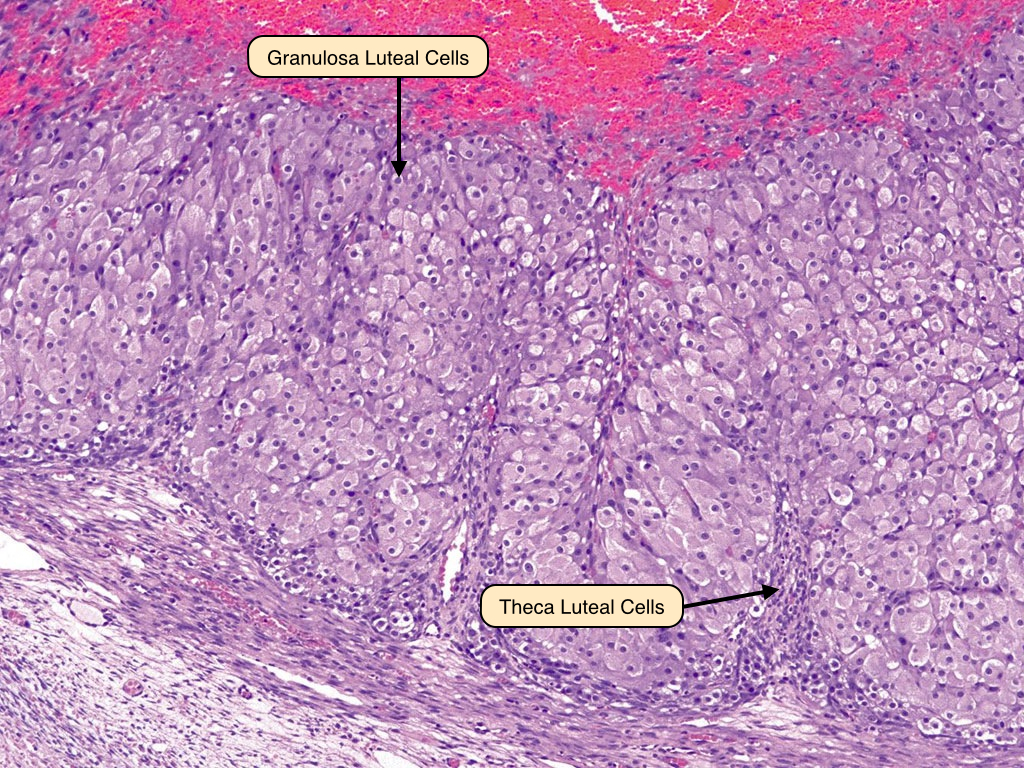
Corpus Albicans
If fertilization does not occur, the corpus luteum involutes to form the corpus albicans that is filled with fibrous tissue. The secretory cells of the corpus luteum degenerate and are phagocytoses by macrophages. 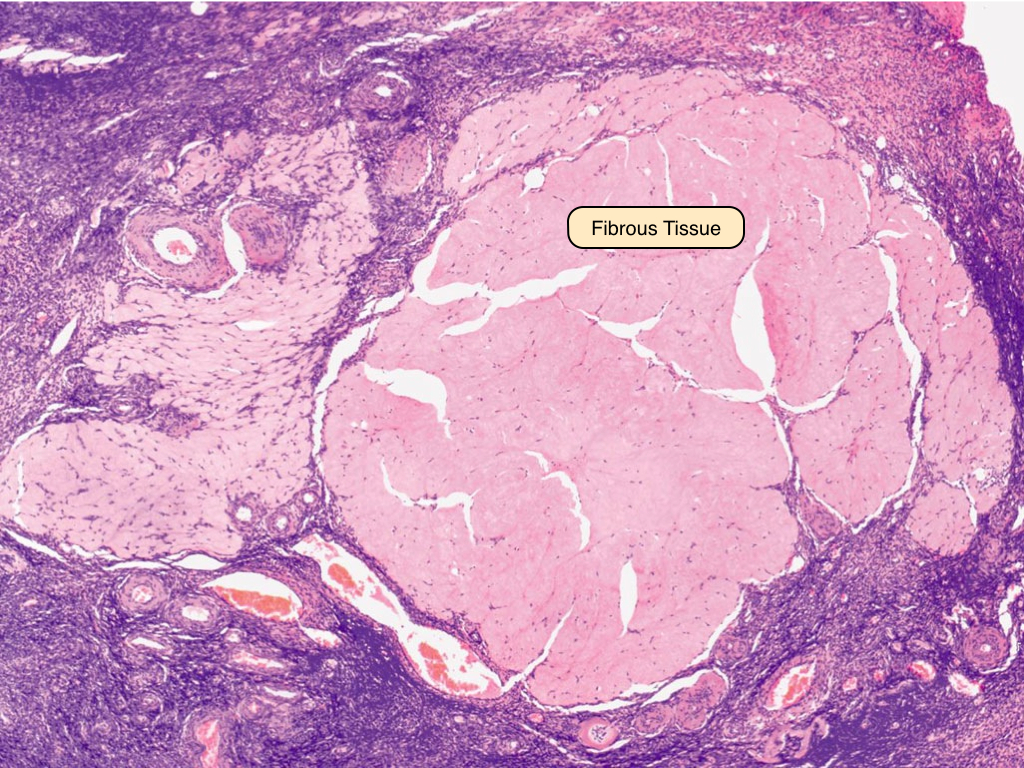
Atretic Follicle
Degeneration of follicle (atresia) can occur at any stage of development. The granulosa cells undergo apoptosis and consequently, the oocyte degenerates. The basement that separated the oocyte from granulosa cells often thickens to become the glassy membrane. Fibrous material replaces the granulosa cells. 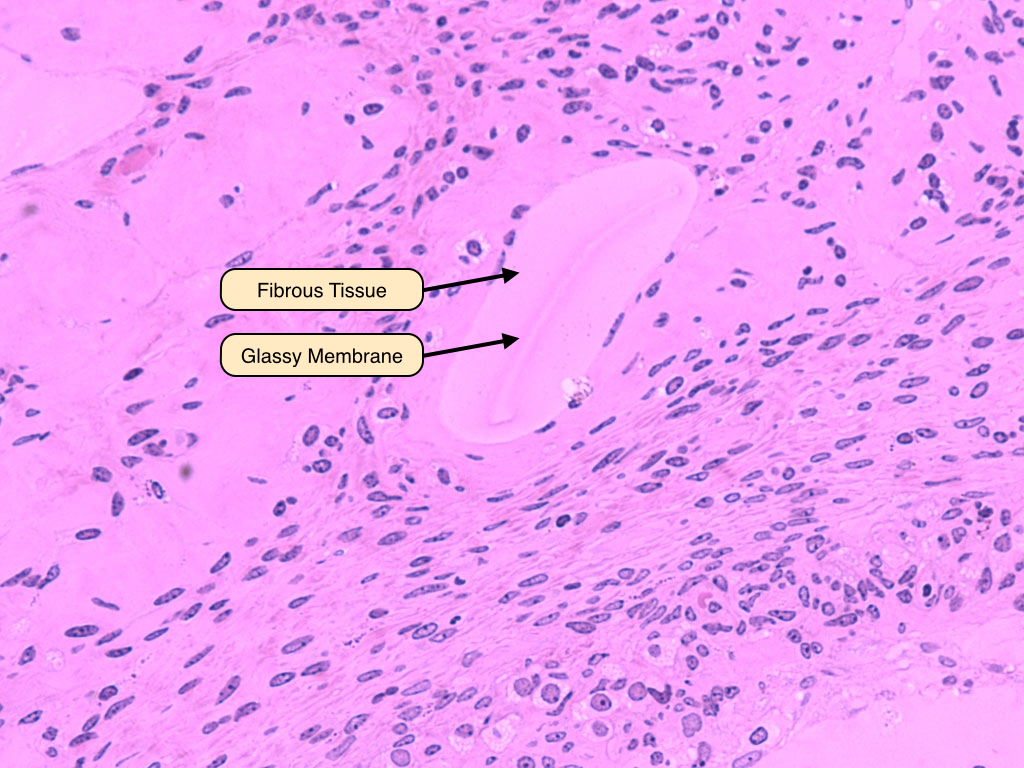
Oviduct
The oviduct consists of several segments: the infundibulum, which contains fimbriae and is located adjacent to the ovary, the ampulla, the isthmus, and the pars interstitialis. The first two of these regions have a characteristic appearance that is dominated by an elaborate mucosa that is thrown into numerous branched folds, surrounded by a relatively thin layer of smooth muscle. As the tube moves away from the ovary and toward the uterus, these folds become smaller and the smooth muscle dominates. 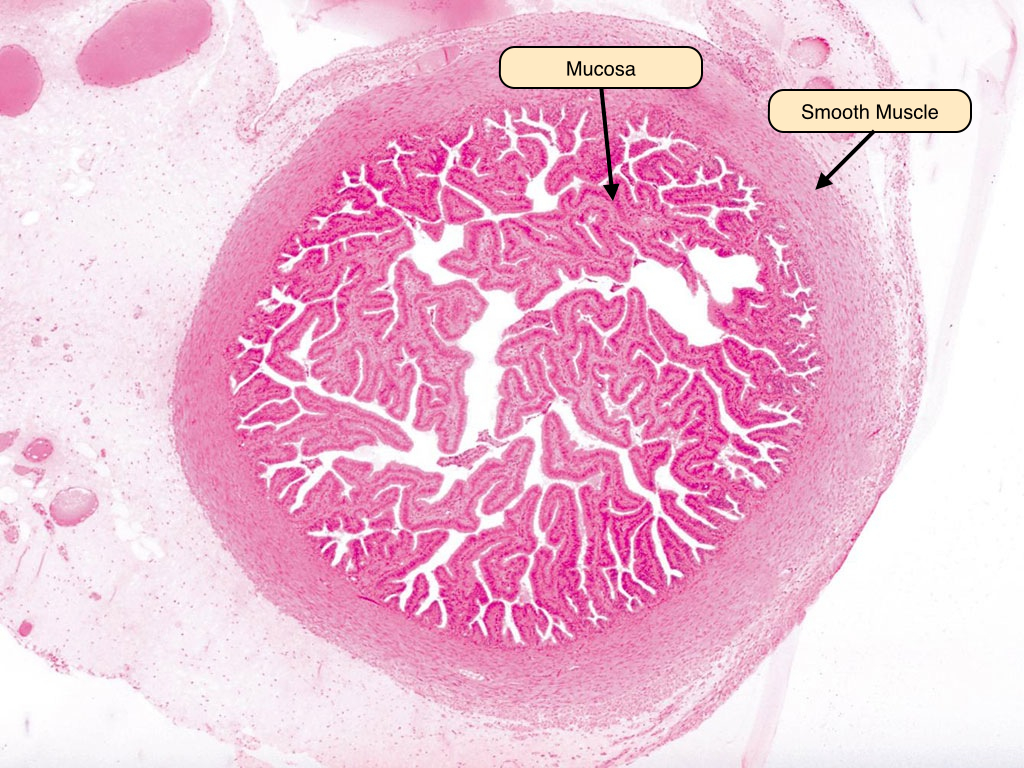
Oviduct Epithelium
The oviduct epithelium consists of two distinct cell types. The ciliated cells dominate and serve to move the ovum away from the ovary and toward the uterus. The non-ciliated secretory cells, also known as peg cells, release a secretion that lubricates the tube and provides nourishment and protection to the traveling ovum. 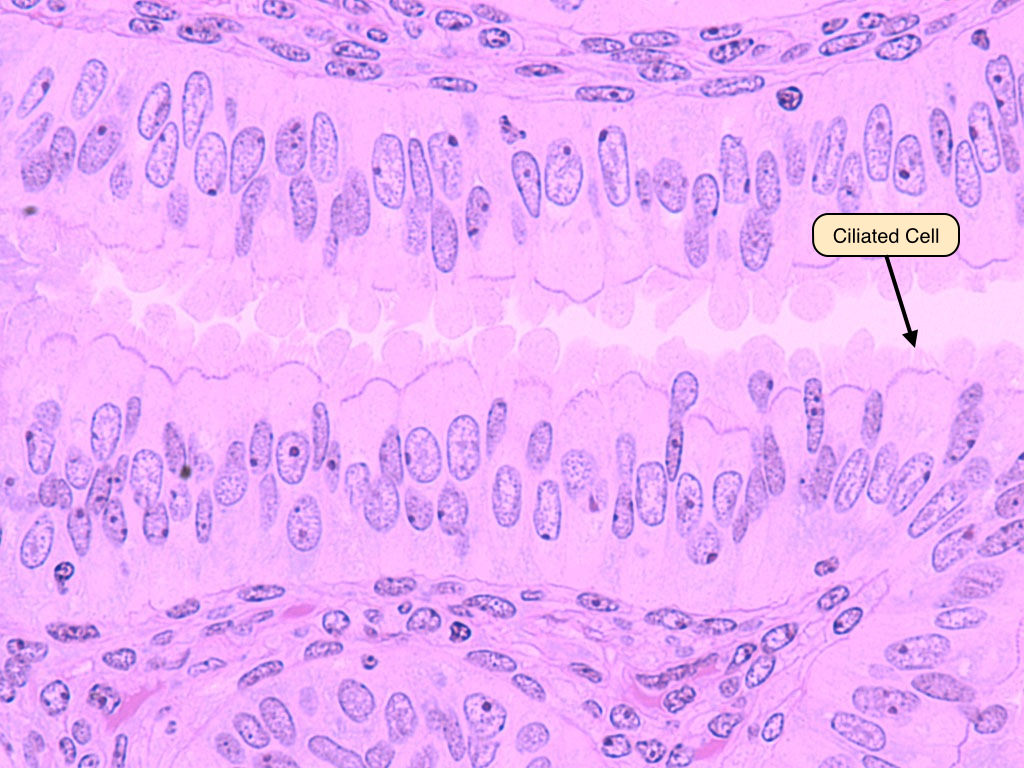
Uterus
The uterus is divided into several layers that have distinct structural and functional characteristics. The simplest classification of these layers is their division into a mucosal layer, or endometrium, a muscularis layer, or myometrium, and a serosal layer, or perimetrium. The endometrium itself is divided into two layers, the stratum functionalis and stratum basalis. During the menstrual cycle, the stratum functionalis expands and vascularizes and is subsequently sloughed off during the process of menstruation, whereas the stratum basalis remains relatively constant. The myometrium allows for the expansion and contraction of the uterine cavity and is responsive to the hormone oxytocin. 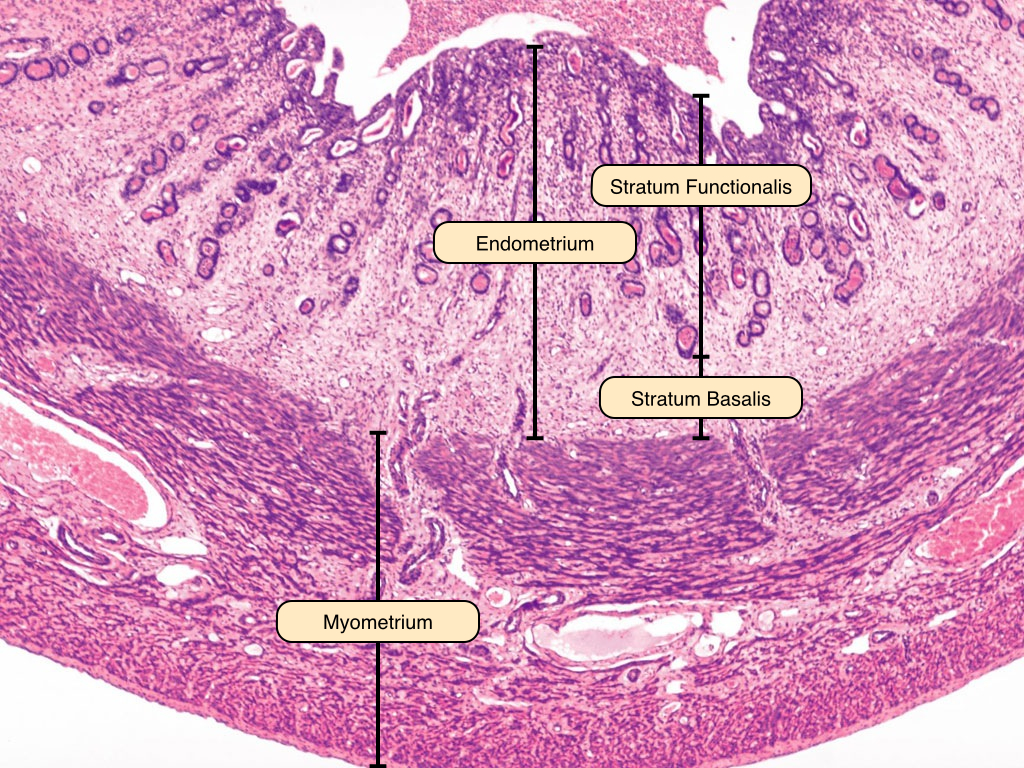
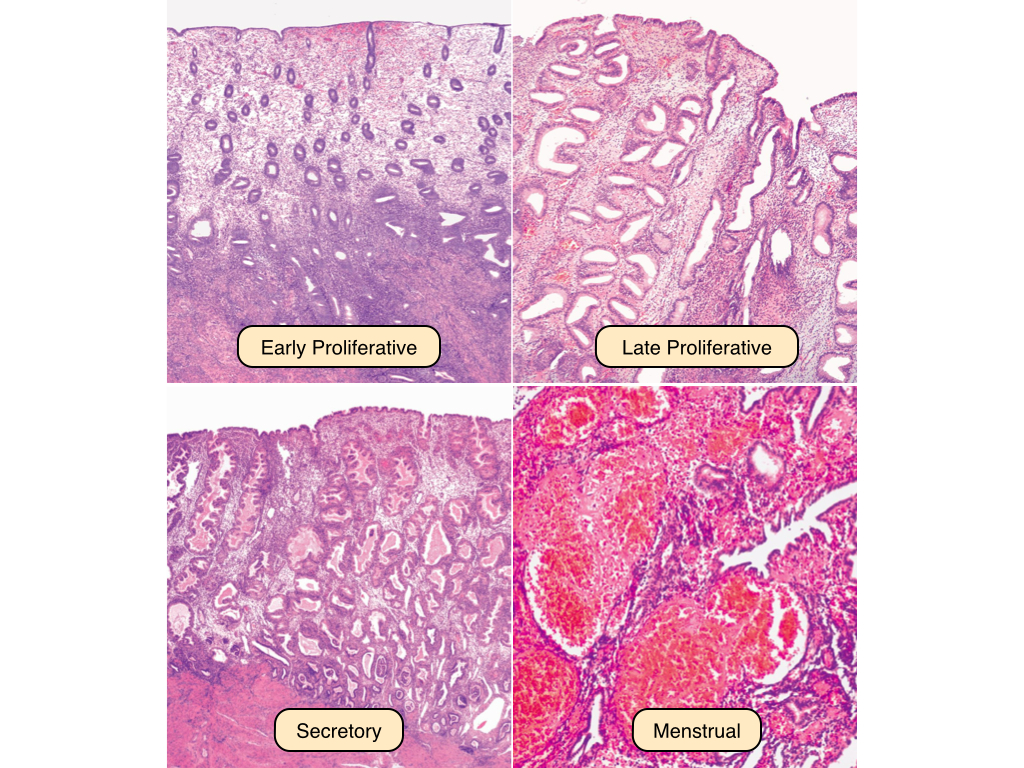
Uterine Cycle
The early proliferative phase of the uterine cycle begins at the end of menstrual flow. The uterine glands in this phase are sparse and relatively small, and the epithelial cells develop microvilli and cilia under the influence of estrogen. The late proliferative phase reveals an increased thickness of the stratum functionalis, and the glands are more coiled and densely packed. The secretory phase of the uterine cycle begins at ovulation. In this phase, the glands become even more complexly coiled and the endometrial lining reaches its maximal thickness, whereas the stratum basalis and myometrium remain relatively unchanged. Note the saw-toothed appearance of the glands. Secretions rich in glycogen and glycoprotein can be observed in the lumina of the glands. If fertilization does not occur, the placental tissue does not produce hCG and the corpus luteum degenerates. The uterine lining does not receive the progesterone, causing the spiral arteries constrict and the endometrial tissue to become ischemic. This causes cell death and the sloughing of the stratum functionalis.
Cervix
The cervix lies at the base of the uterus and serves to protect it from bacterial infiltration. It is the site of an important epithelial transition. The upper cervix (endocervix) is lined by a simple columnar epithelium that contains mucous-secreting cells. In contrast, the lower cervix (ectocervix) is lined by a stratified squamous epithelium. The transition point between these two epithelia is known as the external os. Note how the underlying layers of the cervix are composed primarily of collagenous and elastic connective tissue rather than smooth muscle fibers. 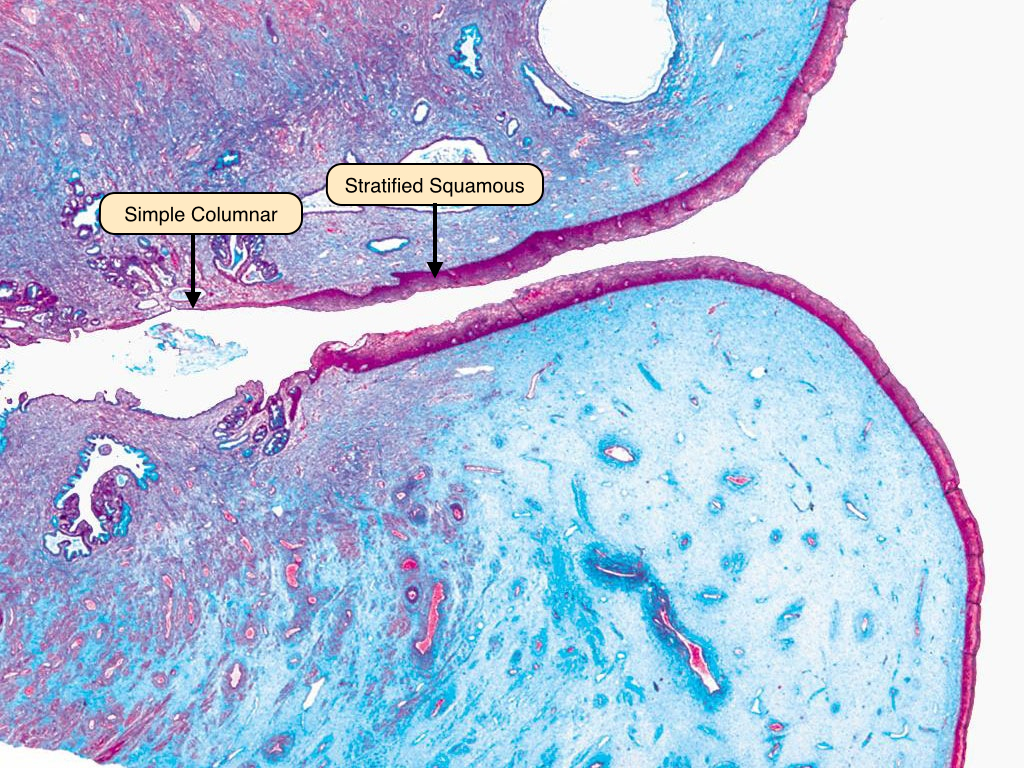
Vagina Epithelium
The vagina is lined by a stratified squamous epithelium that features a small degree of keratinization. Below the epithelium is a thick layer of dense connective tissue, like that in the dermis of the skin. A layer of loose connective tissue containing many blood vessels and nerves follows this. The cells of the vaginal wall typically contain a relatively large amount of cytoplasm because they produce and store glycogen. 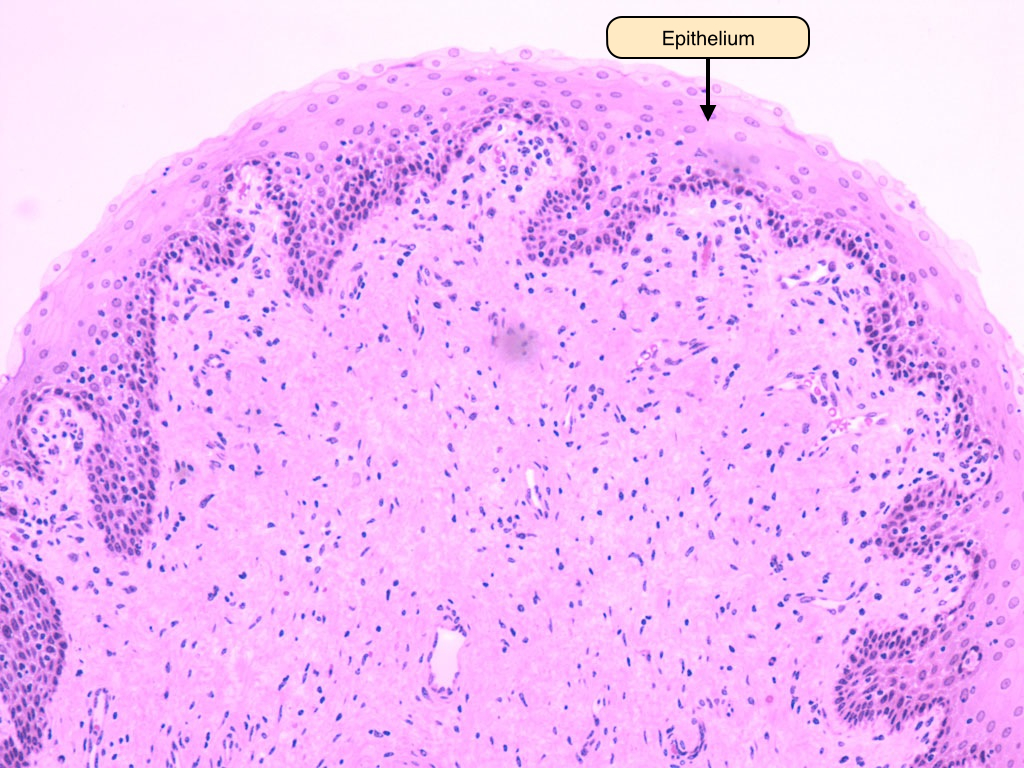


No comments:
Post a Comment