Endocrine System Histology
Endocrine Systems Lab
Learning Objectives
- Describe the organization and function of endocrine tissues, including the key endocrine organs as well as diffuse endocrine cells.
- Distinguish the different types of pituitary cells using the light microscope and electron microscope.
- Name and describe the different layers of the adrenal gland, as well as the blood supply to this gland.
- Contrast the structure of the thyroid with that of the parathyroid.
- Identify islets of Langerhans within pancreatic tissue and explain the relative positions of alpha and beta cells.
Lab Content
Introduction
The term "endocrine" implies secretion into the internal milieu of a multicellular organism. In contrast to exocrine tissues, where the secretory products are discharged into the external space - the outer surface of the body, mucosal surfaces, duct systems - the endocrine organs and cells secrete their products into the vascular system. The blood vessels then serve as conduits for these secretions to travel to their target tissues.
Endocrine tissues function according to a basic model. Individual cell types respond, via surface receptors, to different signals. They produce a very limited spectrum of secretory products, called hormones, that themselves function as signaling molecules for specific cell populations. These hormones are effective at exceedingly low concentrations. Because of this, relatively few cells are sufficient for the integrative function of large, multicellular organisms. Therefore, endocrine tissues are characteristically present in small quantities.
Pituitary Gland
The pituitary gland, or hypophysis, is a collection of different cell types that control the activity of other endocrine organs. It is governed by the hypothalamus, which sends both electrical and hormonal signals to the pituitary, and by feedback regulation (both positive and negative) through the secretions of its target glands. This slide shows a section of the human pituitary. In the anterior pituitary (pars distalis), you can see cords of cuboidal cells with a wide range of nuclear to cytoplasmic volume ratios. The posterior pituitary (pars nervosa) is connected to the hypothalamus by the pituitary stalk - this is easily visualized because the nervous tissue appears continuous between the two glands. 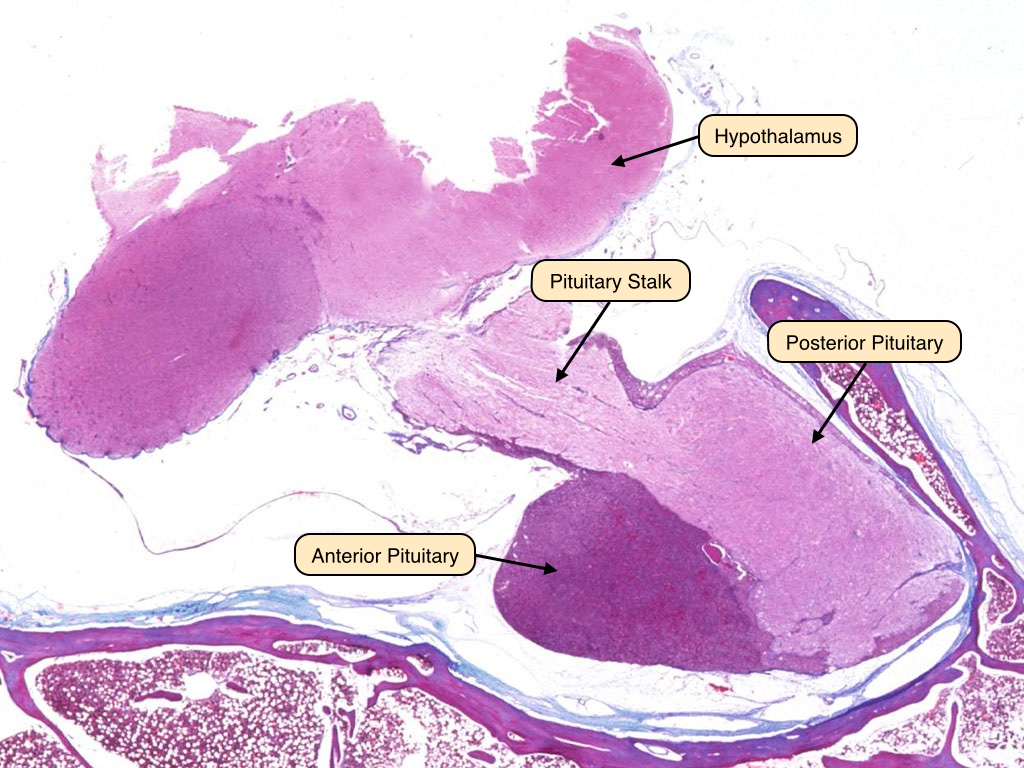
Anterior Pituitary
The anterior pituitary contains cells that, when viewed under the light microscope, appear as acidophils, basophils, or chromophobes. This slide displays the three cell types of the anterior pituitary under H&E stain. The acidophils appear as cells with pink cytoplasm and dark nuclei. These cells secrete protein hormones like growth hormone and prolactin. The basophils appear as darker cells with purple cytoplasm. These cells secrete glycoprotein hormones such as adrenocorticotropic hormone (ACTH), thyroid-stimulating hormone (TSH), follicle-stimulating hormone (FSH), and leutenizing hormone (LH). Finally, a few chromophobes are visible in this section; these cells are non-secretory and serve as support cells or precursors to the acidophils and basophils. 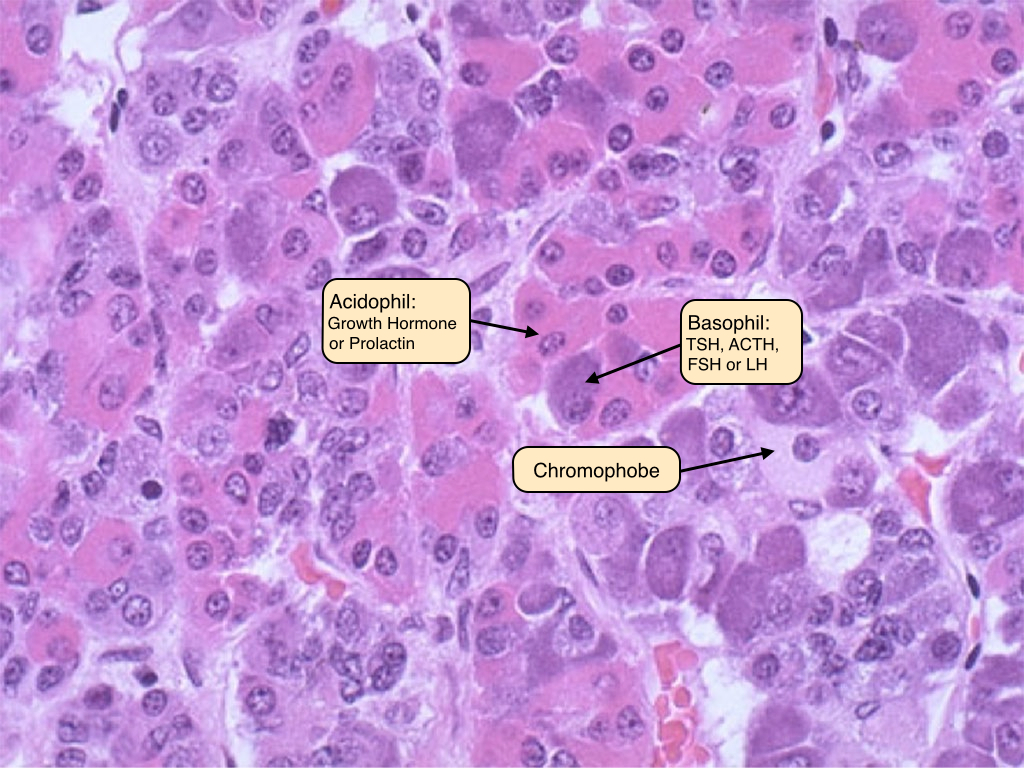
Posterior Pituitary
The posterior pituitary is mostly composed of unmyelinated axonal processes and terminals of the supraoptic and paraventricular nuclei of the hypothalamus. The pituitary stalk connects the two glands. The posterior pituitary has characteristic Herring bodies, focal axonal swellings that are packed with secretory granules. Pituicytes are the glial cells of the pituitary gland; the nuclei that are visible in sections of posterior pituitary belong to these cells, as well as cells of the vasculature. A third section of the pituitary, the intermediate lobe, is vestigial in man. 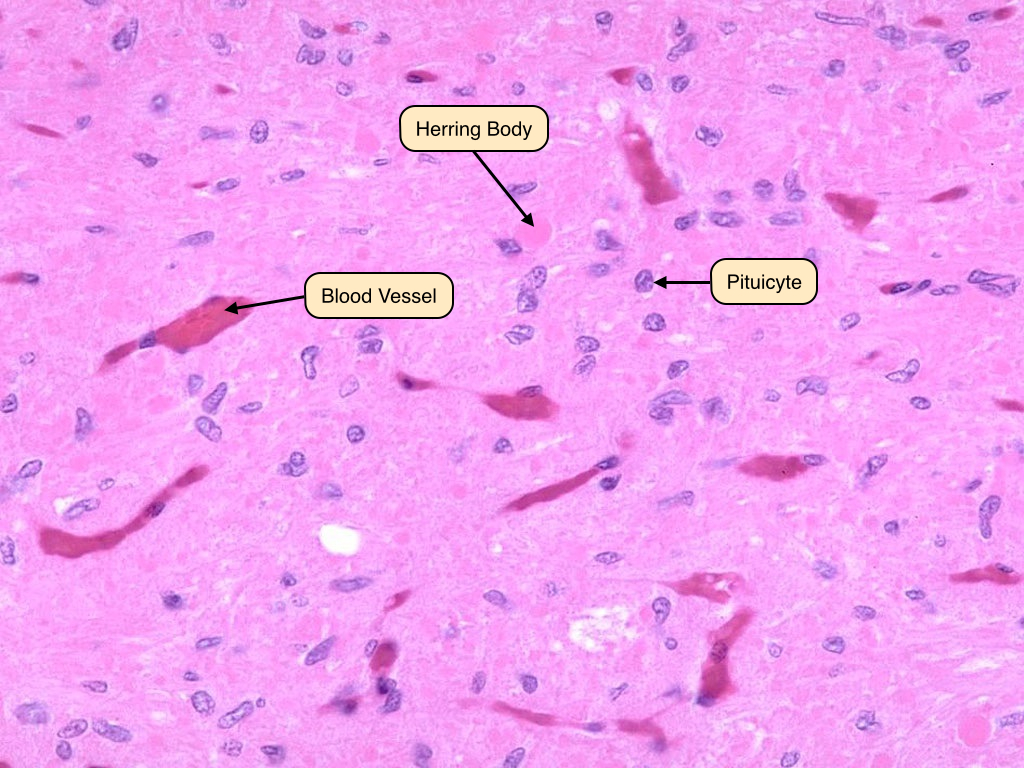
Adrenal Gland
The adrenal gland has two distinct parts, the cortex and medulla, which differ in structure and function. The cortex secretes hormones produced from cholesterol and can be functionally and histologically divided into three zones: glomerulosa, fasciculata, and reticularis. The adrenal medulla is the innermost portion of the gland and shares an embryological origin with the sympathetic nervous system.
The zona glomerulosa is the thin outer layer of the adrenal cortex. Its cells are pale staining and organized in ovoid clusters that are separated by capillaries. The cells of the zona glomerulosa produce mineralocorticoid hormones like aldosterone, which regulates salt and water balance.
The zona fasciculata comprises the thick middle layer of the cortex. Its cells are extensively vacuolated because of the presence of lipid droplets. The cells of this region produce glucocorticoids like cortisol, which has metabolic effects.
The zona reticularis is the innermost layer of the adrenal cortex. The border between it and the zona fasciculata is less distinct than that between the previous two zones. Cells in the zona reticularis stain deeply and are less vacuolated. This region produces androgens, which supplement sex hormones produced by the gonads.
The medulla primarily secretes catecholamines, including adrenaline and noradrenaline. Its cells possess abundant cytoplasmic granules that contain stored peptide hormones and catecholamines. These cells are frequently called chromaffin cells because they can be stained with chromium salts. Preganglionic sympathetic fibers traverse the adrenal cortex and synapse directly on chromaffin cells, where they release acetylcholine to stimulate the exocytosis of catecholamine granules during a sympathetic response. 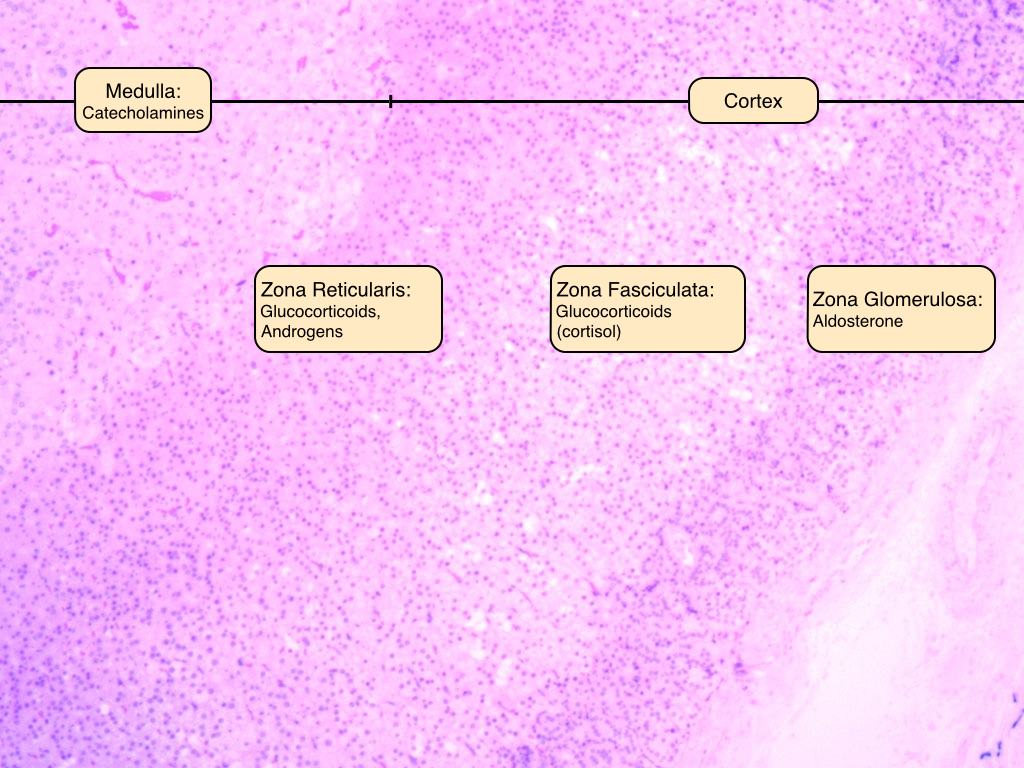
Thyroid
The thyroid is located in the neck and stores large amounts of inactive hormone within extracellular compartments. The thyroid consists of structural units called follicles, which are composed of secretory epithelial cells called principal cells that are adjoined by junctional complexes and surrounded by a basement membrane. Follicles vary in size, but each displays a central lumen containing colloid. Colloid consists of the glycoprotein thyroglobulin, which is secreted by the principal cells and serves as a precursor to thyroid hormone. The height of the principal cells varies according to their level of secretory activity; in hypothyroidism, the cells are squamous or cuboidal, whereas in hyperthyroidism, they are columnar.
Also visible in this slide are a few C-cells, or parafollicular cells, scattered in the spaces between follicles. C-cells secrete calcitonin, which serves as a fine control for calcium homeostasis. 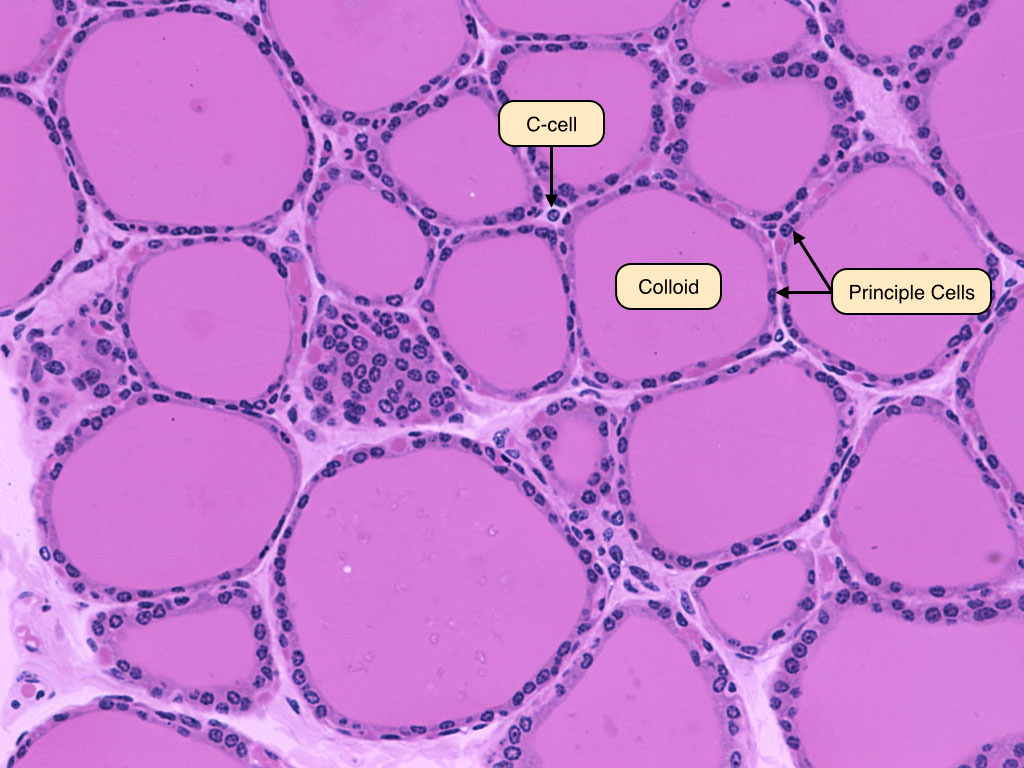
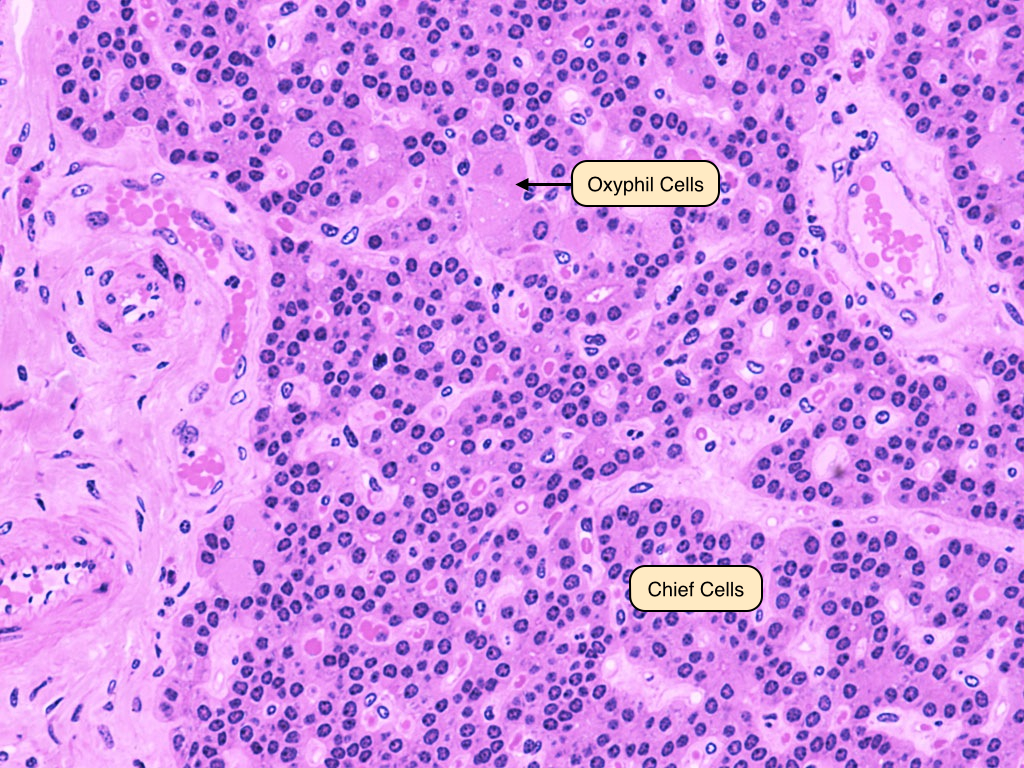
Parathyroid
The parathyroid glands are closely associated with the thyroid. They consist of closely packed groups of two cell types:
- Chief (principal) cells, which have prominent central nuclei surrounded by pale cytoplasm. Chief cells produce parathyroid hormone (PTH), which is the most important regulator of calcium metabolism in humans.
- Oxyphilic cells, which are large and fewer in number, have small, dark nuclei and an acidophilic cytoplasm with many mitochondria. The function of these cells is unknown, but they increase in abundance as a person ages.
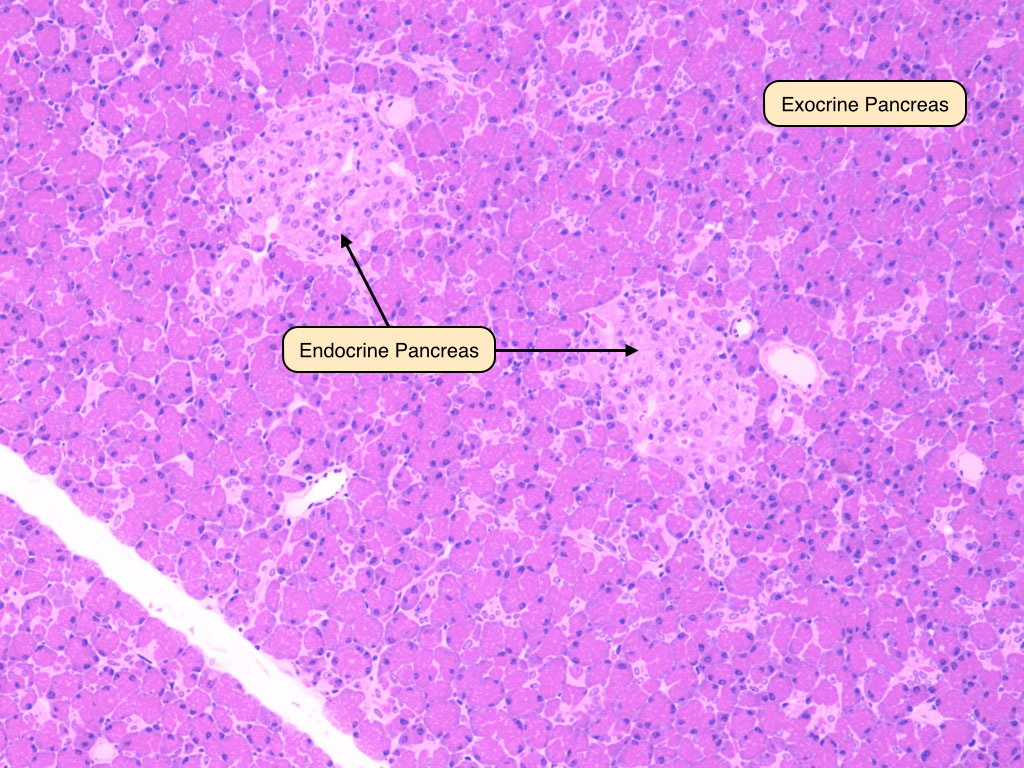
Endocrine Pancreas
The endocrine portion of the pancreas is comprised of the islets of Langerhans. During development, the cells of the islets migrate away from the duct system and aggregate around capillaries. The islets contain three important cell types:
- Alpha cells produce glucagon, which increases the plasma glucose concentration. They are primarily located around the periphery of the islets.
- Beta cells produce insulin, which decreases plasma glucose by promoting uptake by liver, skeletal muscle, and adipose tissue. Beta cells are typically located in the center of the islets.
- D-cells produce somatostain, which has broad effects on gastrointestinal function and inhibits insulin and glucagon secretion. Delta cells are scattered throughout the islets.


No comments:
Post a Comment