Urinary System Histology
Urinary System
Learning Objectives
- Distinguish the key microscopic components of the renal cortex and medulla
- Identify the structural components of the nephron
- Describe the structure of the surface across which filtration occurs
- Identify and distinguish the proximal tubule, distal tubule, and collecting duct
- Identify the component cells of the juxtaglomerular apparatus
- Name the important histological characteristics of the ureter, bladder, and urethra
Lab Content
Introduction
The urinary system is comprised of the kidney, ureter, urinary bladder, and urethra. The kidney produces urine, which contains excess water, electrolytes and waste products of the body. It then flows down the ureter into the bladder where it is temporarily stored. The bladder is then emptied via the urethra.
The kidney has several important homeostatic, hormonal, and metabolic functions that include:
- The maintenance of water and electrolyte homeostasis
- Regulation of acid-base balance in conjunction with the respiratory system
- Excretion of metabolic waste products, especially the toxic nitrogenous compounds
- Production of renin for blood pressure control and erythropoietin, which stimulates red blood cell production in the bone marrow
- Conversion of vitamin D into active form for the regulation of calcium balance
Kidney
This is a low power view of a cross section through the kidney. The kidney is composed of an outer cortex and inner medulla. Note the inner medullary tissue surrounded by the outer cortical tissue. The cortical section contains glomeruli, tubules, blood vessels and medullary rays. The medullary primarily contains loops of Henle, collecting ducts and blood vessels. 
Nephron
The nephron is the functional unit of the kidney. There are about two million nephrons in each kidney. Nephrons begin in the cortex as corpuscles; become tubules and dip down to the medulla; then return to the cortex before draining into the collecting duct. The collecting ducts then descend towards the renal pelvis and empty urine into the ureter.
The components of a single nephron include:
- renal corpuscle
- proximal convoluted tubule
- loop of Henle
- distal convoluted tubule
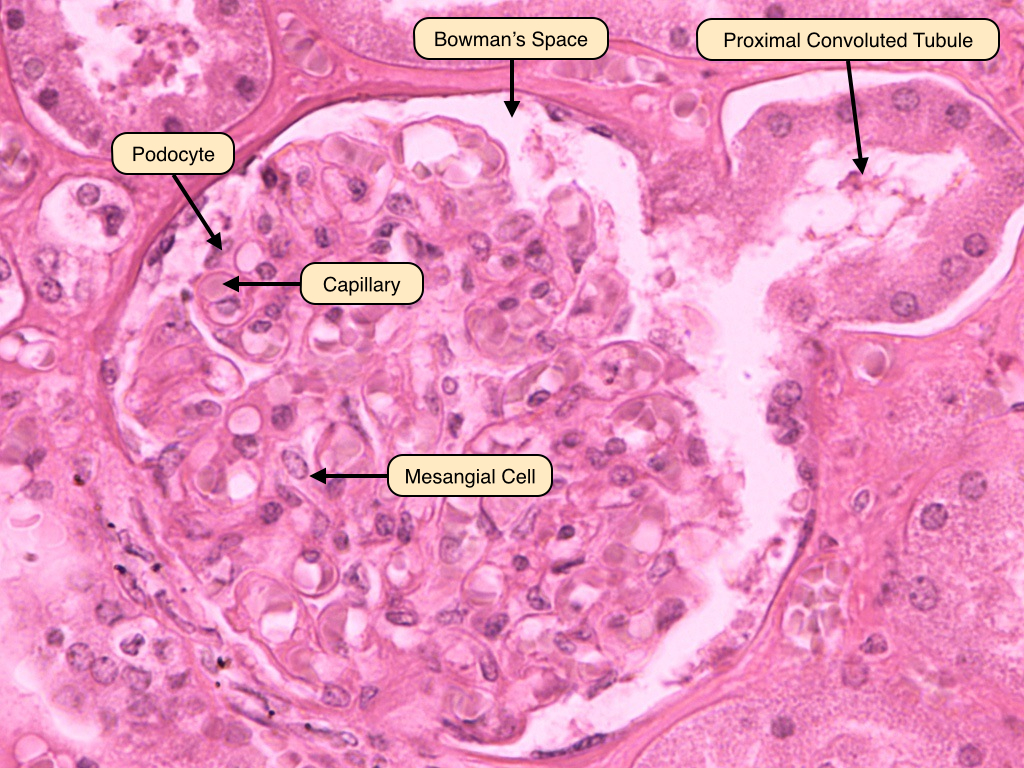
Renal Corpuscle
The renal corpuscle is where plasma is filtered from capillaries into the renal tubules. At the center of renal corpuscle is the glomerulus, a meshwork of capillaries. Bowman's capsule surrounds the glomerulus. The space in between Bowman's capsule and the glomerulus is called Bowman's space and is where the ultrafiltrate of plasma is first collected. Also note the vascular pole of the renal corpuscle; this is the location where afferent arterioles become efferent arterioles. On the opposite end of the vascular pole lies the urinary pole where plasma ultra-filtrates exits Bowman's capsule and enters the proximal convoluted tubule.
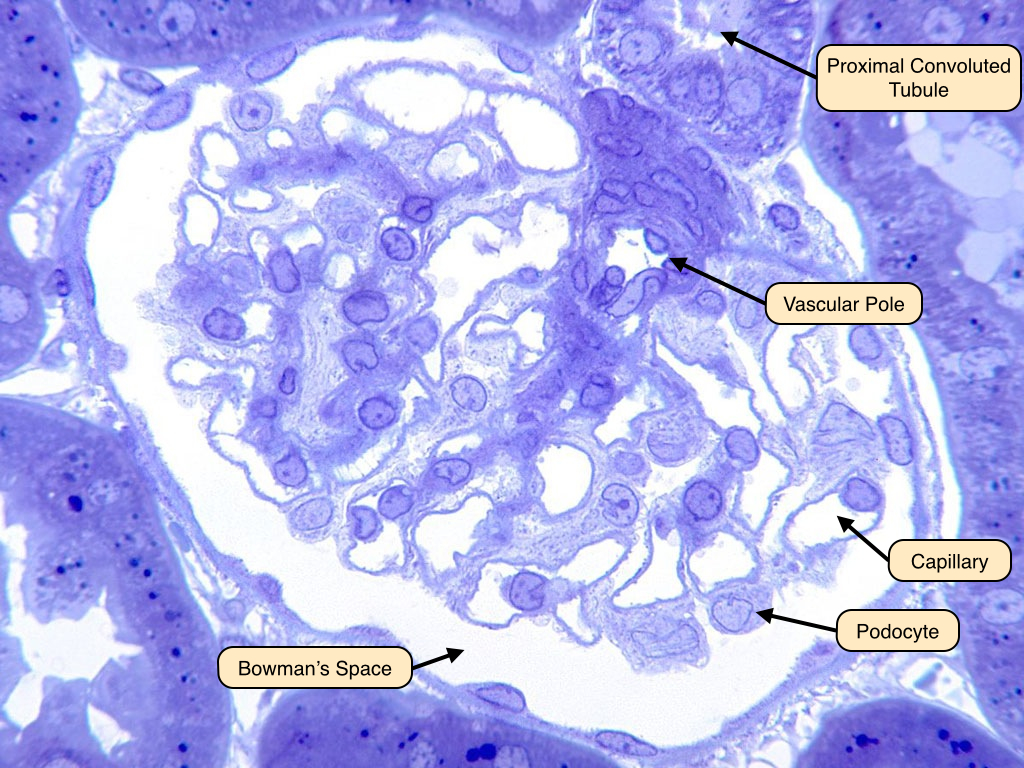
Renal Corpuscle 2
In this image toluidine blue was used to stain the glomerulus. Toluidine blue stains nucleic acids and polysaccharides blue or purple and is effective for labeling the basement membrane in the glomerulus. Mesangial cells are responsible for synthesizing the basement membrane-like material that supports the structure of the glomerulus. They can be easily identified by their prominent nuclei within the glomerulus. Note how the podocytes lie between the capillaries and Bowman's space. The plasma has to pass through a filtration barrier of three layers to enter Bowman's space: the capillary endothelium, the podocyte layer, and their fused basement membrane.
Podocytes EM
Podocytes are specialized eptithelial cells that separate the network of capillaries in the glomerulus from Bowman's space. Podocytes extend processes that surround the capillaries. These processes form secondary processes called foot processes. The foot processes associate with the basement membrane opposite from the endothelial cells of the capillaries. 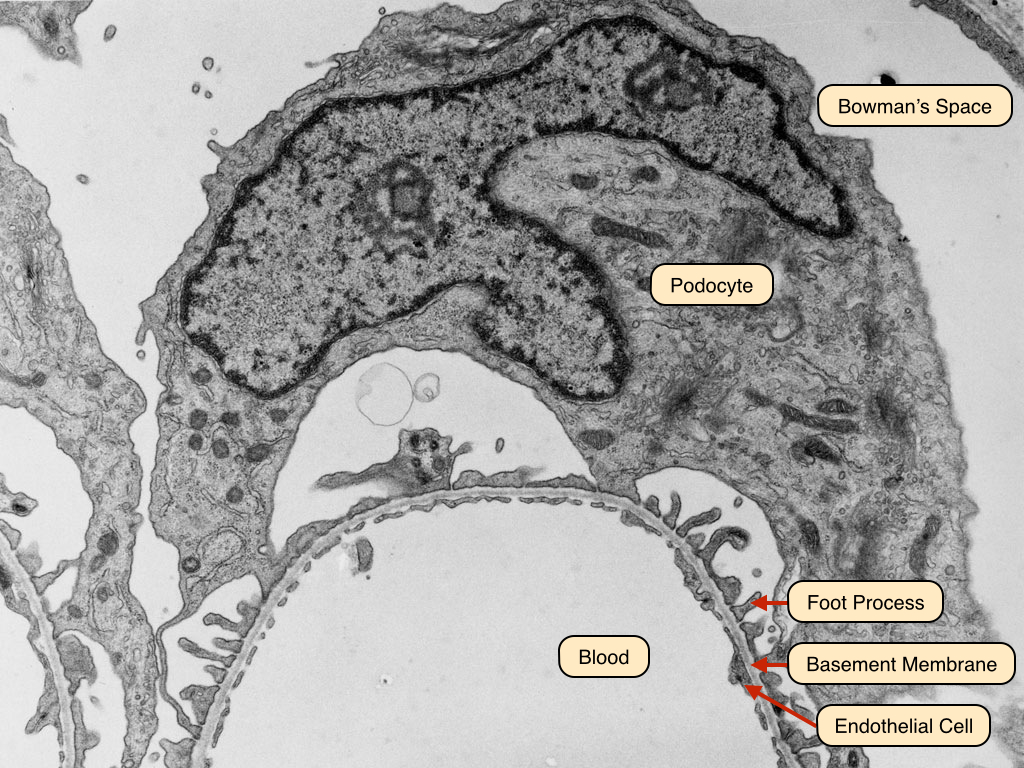
Filtration Barrier
The filtration barrier of the glomerulus consists of a fenestrated capillary epithelium with a negatively charged surface that repels many plasma proteins. Beneath the capillary epithelium is a thick basement membrane that is also negatively charged. The foot processes of the pododcytes form the final barrier. Note the slit diaphragm between the foot processes. These play a role in filtration of plasma as mutations in genes that encode proteins of slit diaphragms lead to proteinuria. 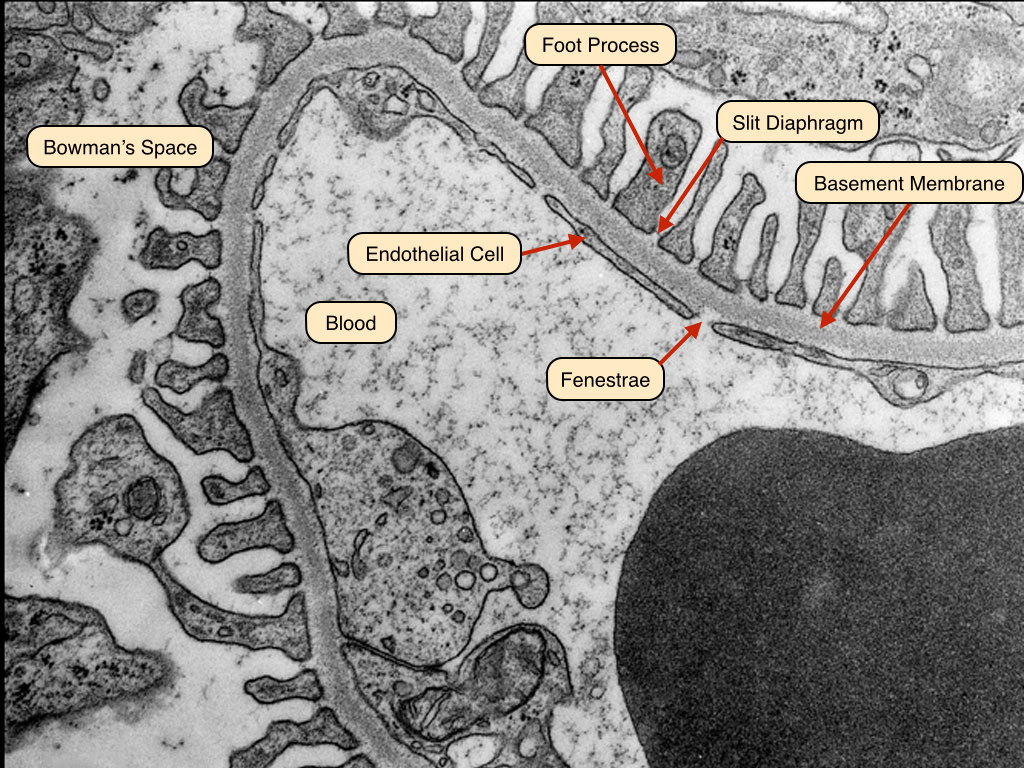
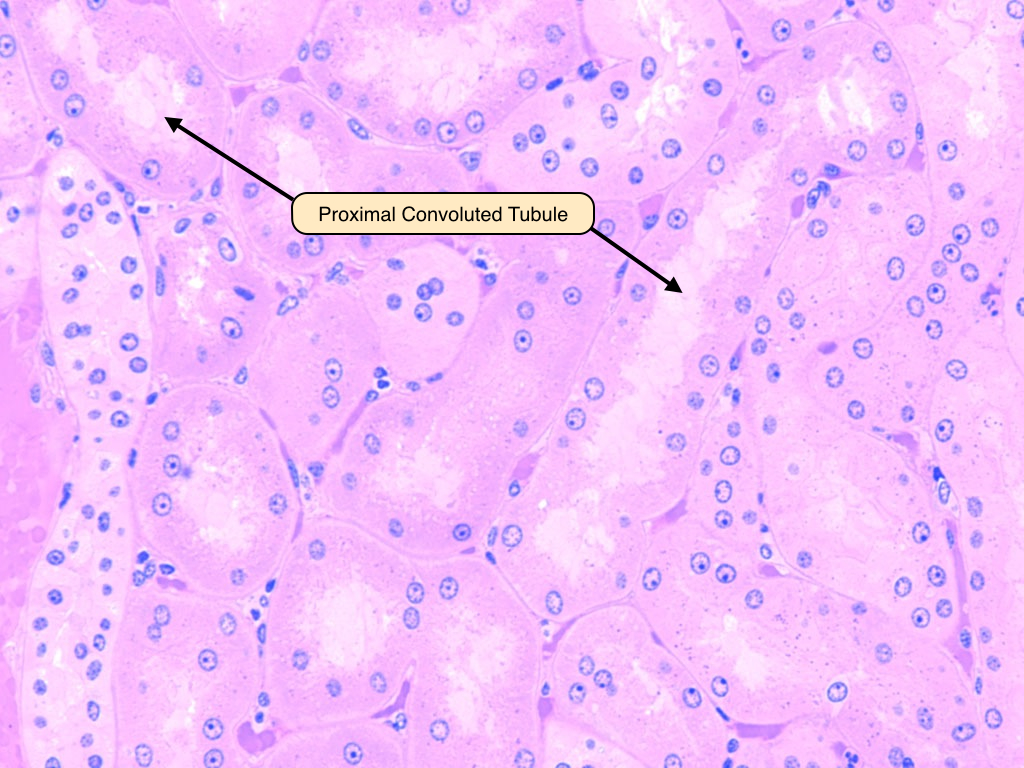
Proximal Convoluted Tubule
The proximal convoluted tubule is the site where majority (65%) of ions and water in the urinary space is reabsorbed back into the body. The cells of the proximal convoluted tubule have a deeply stained, eosinophilic cytoplasm. The cells are large so that in cross section not every nucleus will be visible, making it appear that the proximal convoluted tubule has fewer nuclei than other tubules. The cells also have an apical brush border to increase their surface area.
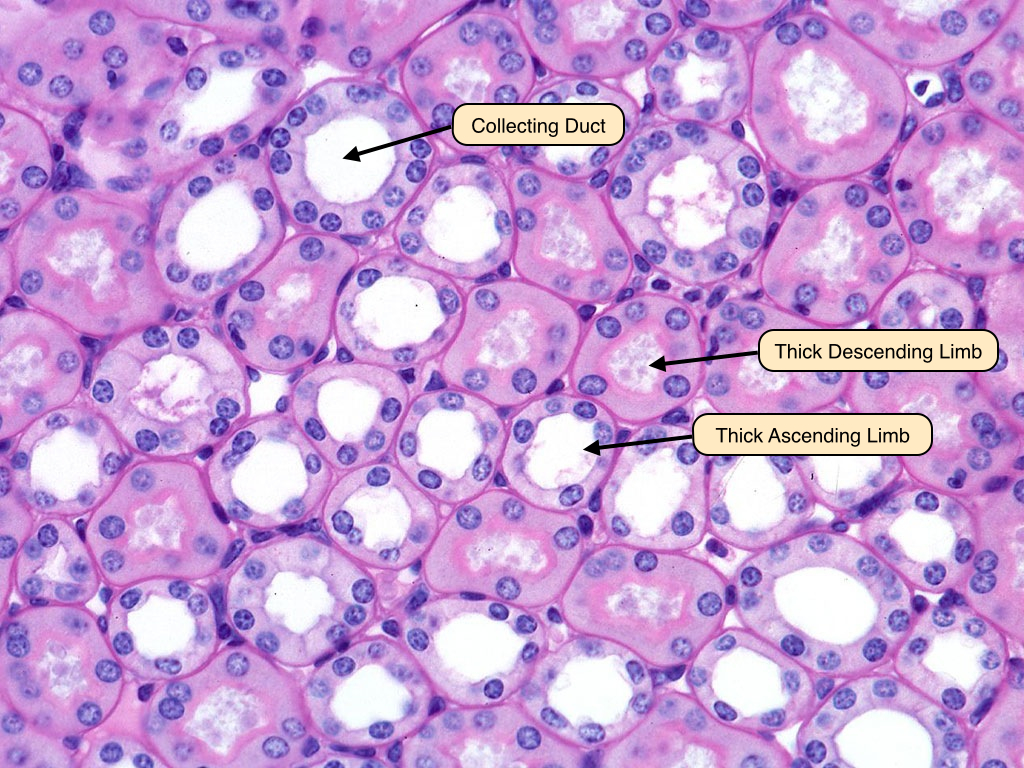
Loop of Henle
The loop of Henle forms a hair-pin structure that dips down into the medulla. The turn of the loop of Henle usually occurs in the thin segment within the medulla, and the tubule then ascends toward the cortex parallel to the descending limb. The thick descending limbs of the loop of Henle look similar to the proximal tubule, with apical brush borders. The thick ascending limbs are composed of cuboidal cells, but unlike the proximal convoluted tubule, they do not have apical brush borders. Collecting ducts can also be seen on this slide. They can be easily distinguished by the presence of prominent lateral borders between adjacent cells.
Distal Convoluted Tubule
The cells of the distal convoluted tubule are smaller and more lightly stained than those of the proximal convoluted tubule. Consequently, more nuclei are apparent in a cross section of distal convoluted tubule compared to proximal convoluted tubule. Distal convoluted tubules also lack a brush border on their apical surface. Note that in any given section of the kidney cortex, much less space is occupied by distal convoluted tubules as compared to proximal convoluted tubules. This is simply because the distal convoluted tubule is shorter and less convoluted. 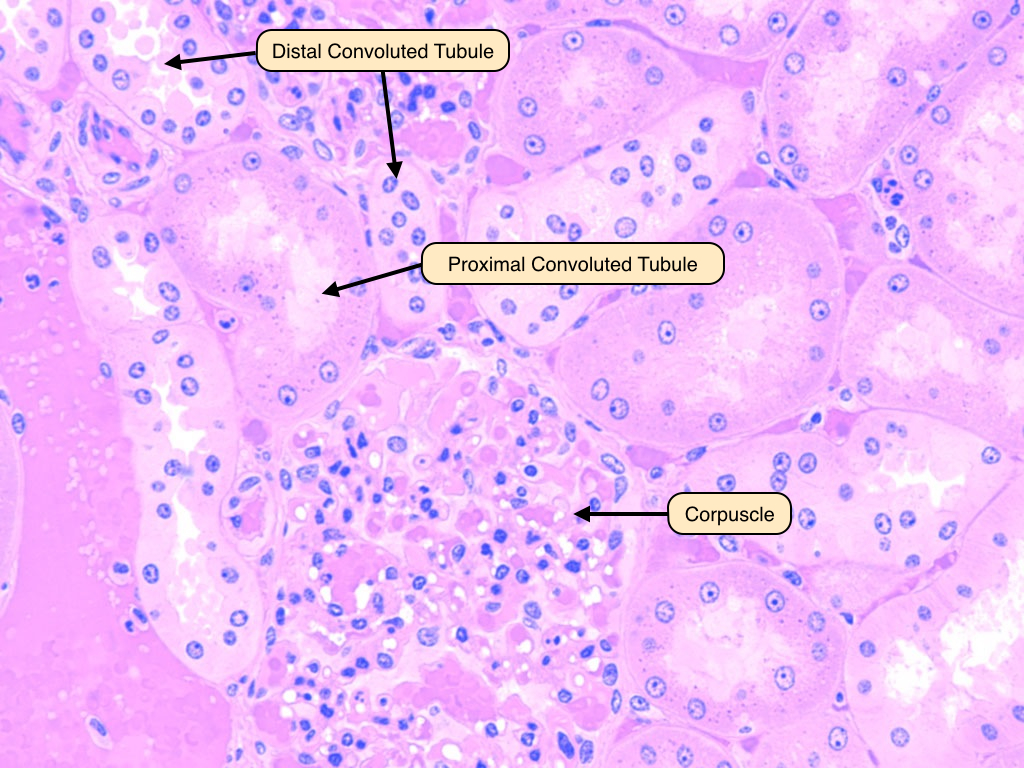
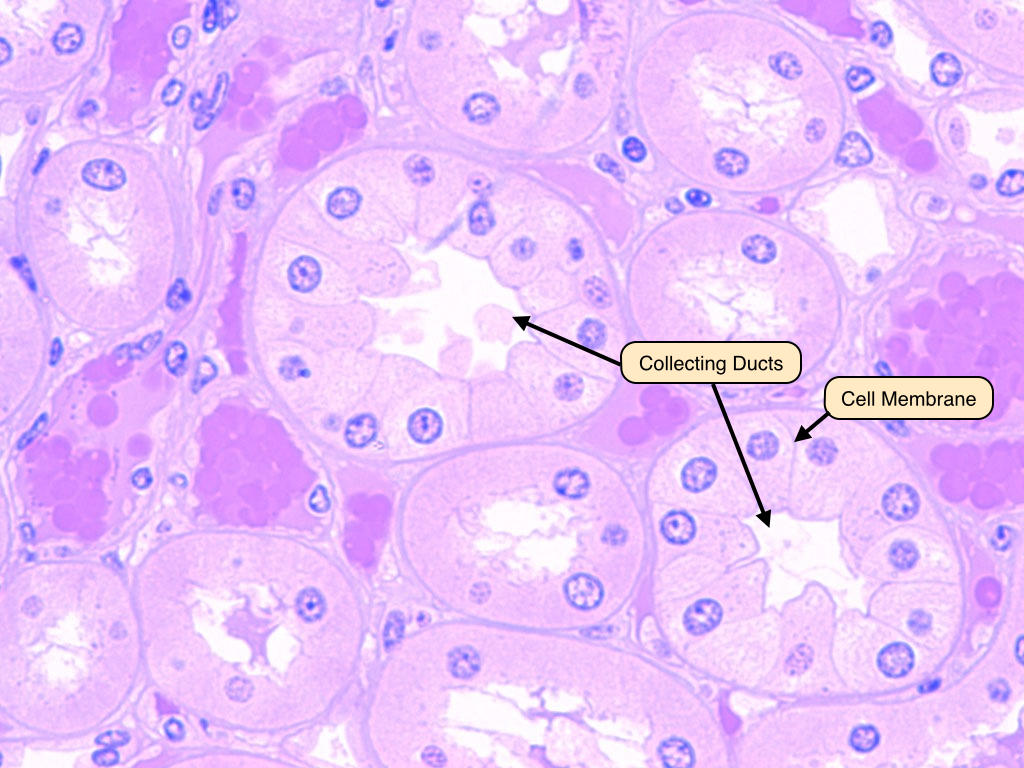
Collecting Ducts
The terminal portion of the distal tubule empties through collecting tubules into a straight collecting duct in the medullary ray. Collecting ducts can be differentiated from other tubules by the prominent lateral borders of the epithelial cells. The collecting duct system is under the control of antidiuretic hormone (ADH). When ADH is present, the collecting duct becomes permeable to water. The high osmotic pressure in the medulla then draws out water from the renal tubule.
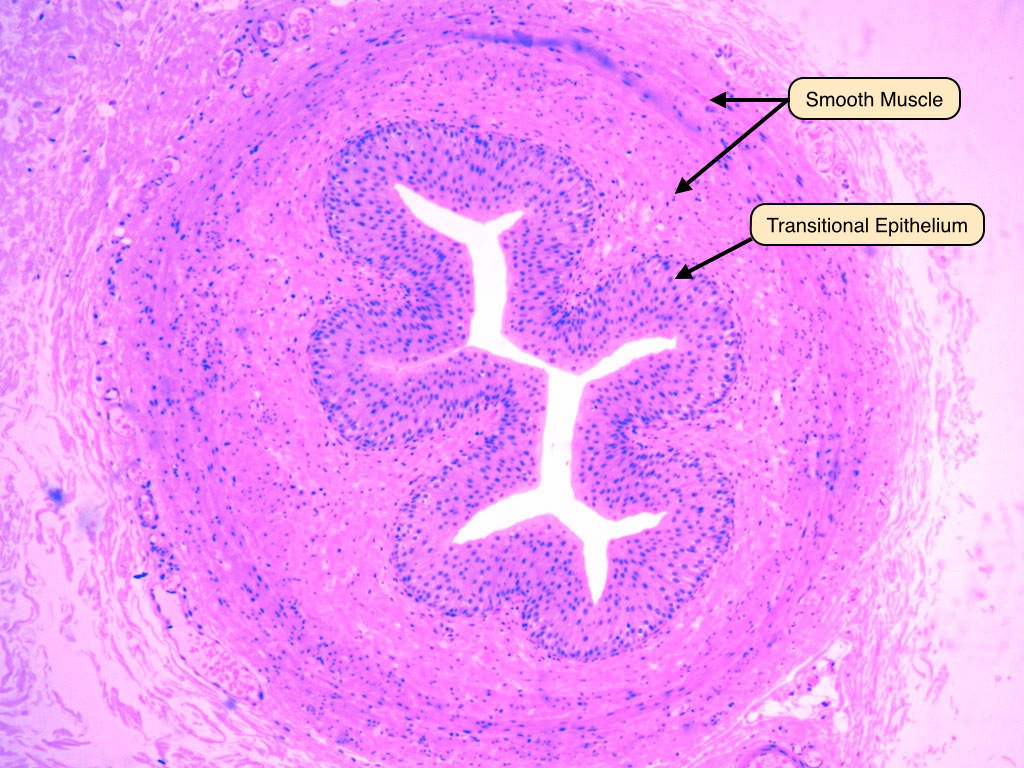
Ureter
The ureter connects the kidney and the urinary bladder. The ureter is a muscular tube, composed of an inner longitudinal layer and an outer circular layer of smooth muscle. The lumen of the ureter is covered by transitional epithelium (also called urothelium). Recall from the Laboratory on Epithelia that the transitional epithelium is unique to the conducting passages of the urinary system. Its ability to stretch allows the dilation of the conducting passages when necessary.
Urinary Bladder
The urinary bladder is lined by transitional epithelium, underneath which are thick layers of smooth muscle interwoven in various directions. This image shows a relaxed bladder where the epithelial cells appear cuboidal. In a distended bladder the epithelial cells are stretched and become more squamous. 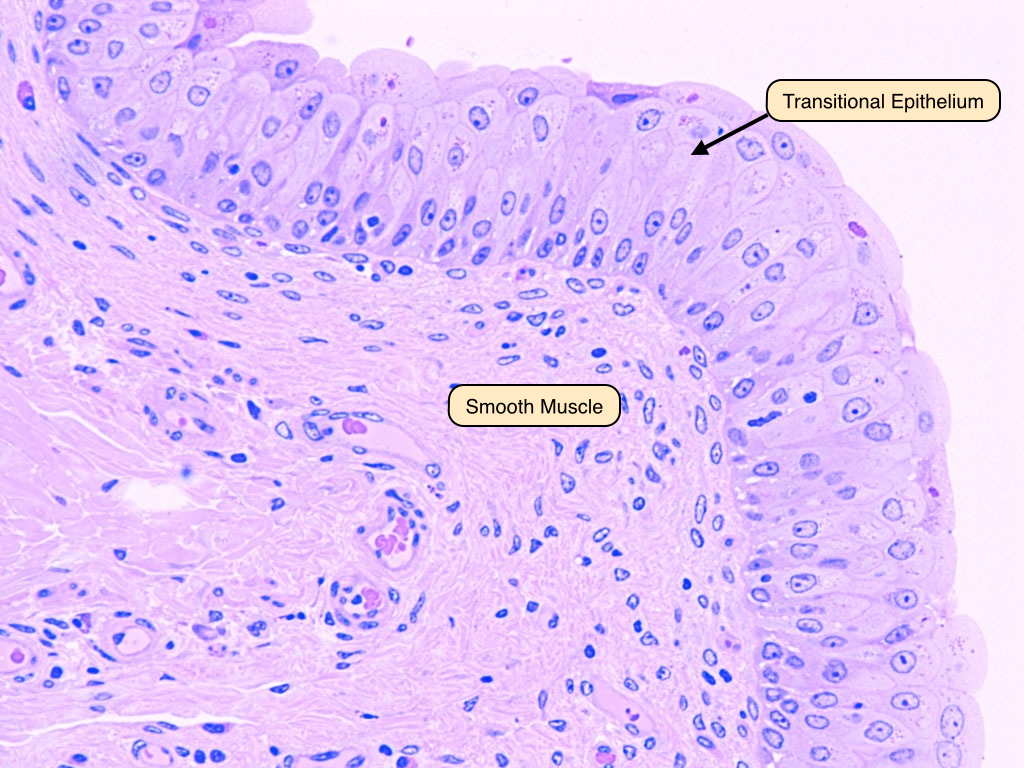


No comments:
Post a Comment